Brain sphingolipid metabolism is closely involved in Gaucher disease
Neurodegenerative disorders affect millions worldwide. Research on these conditions has largely focused on perturbations in protein metabolism. However, there is emerging evidence that disruptions in lipid metabolism – particularly those that perturb the synthesis or breakdown of sphingolipids – also contribute significantly to the progressive neuronal toxicity observed in neurodegeneration.

“In this path-breaking study we have uncovered many previously unknown aspects of how sphingolipids are regulated,” said corresponding author Dr. Hugo J. Bellen, distinguished service professor of molecular and human genetics at Baylor College of Medicine and investigator and chair in neurogenetics at the Jan and Dan Duncan Neurological Research Institute at Texas Children’s Hospital. “Our study reveals a close relationship between sphingolipid metabolism and rare as well as common neurological conditions. Moreover, it offers valuable insights into the molecular cause of Gaucher disease that have opened new avenues to develop potential therapies for this and several other neurodegenerative disorders, including Parkinson’s disease.”
Accumulation of glucosylceramide leads to Gaucher disease
Proteins and lipids are broken down by enzymes in intracellular structures or organelles called lysosomes, which serve as cellular trash compactors or recycling centers. Any perturbations in this cleanup process allows metabolic waste products to accumulate in the lysosomes, which can cause a progressive degeneration of neurons, brain cells that are particularly vulnerable to lysosomal dysfunction.
Gaucher disease is a rare metabolic and lysosomal storage disorder that affects approximately 6,000 individuals in the United States. These individuals have a mutation in the Glucosylceramides Beta (GBA1) gene that encodes the enzyme glucocerebrosidase that catalyzes the conversion of a sphingolipid called glucosylceramide (GlcCer) to ceramide. In the absence of this enzyme, GlcCer accumulates in various organs including the brain, liver, bone marrow and spleen.
Neuronal activity triggers the production of glucosylceramide
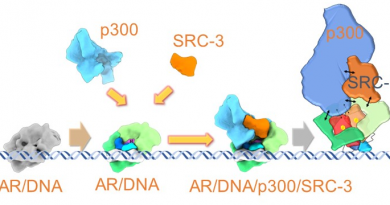
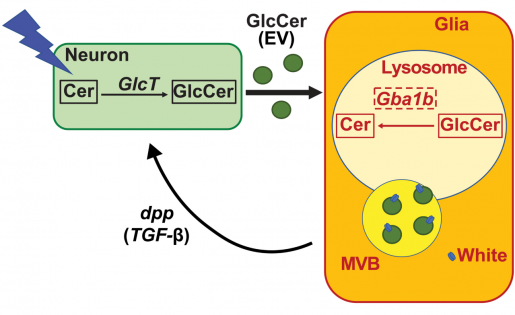
“To tease apart the precise molecular mechanisms underlying GlcCer accumulation we undertook a detailed analysis of the Gba1b gene, the fly homolog of the human GBA1 gene,” said Dr. Liping Wang, a freshly graduated Ph.D. student in the Bellen lab and first author of the study. “Interestingly, we found that under normal conditions, the protein encoded by this gene is expressed exclusively in glia. We then found that also under normal conditions, neurons synthesize GlcCer using ceramide glucosyltransferase, an enzyme that is encoded by GlcT. GlcCer is then broken down into ceramide by the enzyme encoded by Gba1b in glia. Hence, GlcCer needs to be transported from neurons to glia for degradation.”
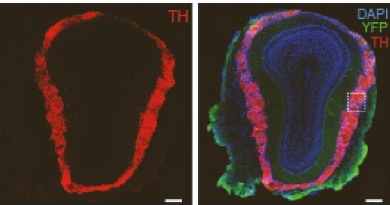
The researchers investigated this metabolic path in fruit fly eyes, a well-established model to study neurodegeneration. The visual system of the flies consists of hundreds of highly organized structures called ommatidia, which have eight photoreceptor neurons arranged in a circular fashion surrounded by pigment and cone glial cells. This arrangement supports the structure and function of photoreceptor neurons.
Using a co-culture system and monitoring the movement of fluorescently-labeled GlcCer, the team showed that GlcCer is transported from neurons to glia.
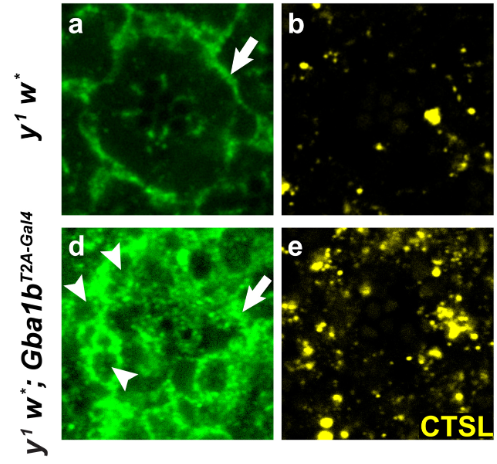
To assess how the loss of Gba1b gene leads to morphological and functional defects in the neurons and glia, Liping and her colleagues generated flies that lacked the Gba1b gene. First, they showed that Gba1b is required in glia and is sufficient to support neuronal function. Liping then examined the localization and levels of Gba1b’s substrate, GlcCer in the fly eye by exposing adult flies to a 12-hour dark/light cycle. “In normal flies, light stimulation promoted a strong increase in the levels of GlcCer both in neurons and in the pigment glia,” Liping said.
We observed similar increases in GlcCer levels in various parts of the brain, indicating that neuronal activity triggers GlcCer synthesis in the central nervous system, which is an exciting finding. This is the first study to associate neuronal activity to sphingolipid levels.”
Gba1b in the glia supports the function of nearby neurons and regulates GlcCer levels
The researchers observed that loss of Gba1b leads to a vast increase in lysosomes in the glia along with progressive accumulation of GlcCer in these cells and obvious signs of a glial demise followed by neurodegeneration. Moreover, they found a transmembrane transporter known as White promotes the transport of GlcCer to glial lysosomes. Their data suggest that while GlcCer accumulation is toxic in both cell types, the structure and function of glia are impacted first and this is followed by the functional loss of neurons.
Finally, they discovered that the protein signaling pathway in the glial cells called the transforming growth factor-beta/bone morphogenetic (TGF-beta/BMP) induces the transport of GlcCer from neurons to glia via small structures called exosomes. The Bellen team also verified that cell lines derived from human tissues employ similar mechanisms to regulate sphingolipid levels.
Together, these novel findings provide the first comprehensive demonstration of how neuronal activity and a cross-talk between neurons and glia regulate sphingolipid and ceramide metabolism to contribute to Gaucher’s disease. “This has also implications for several other neurodegenerative conditions including lysosomal storage disorders and Parkinson’s disease,” Bellen said. “We are excited by the possibility of targeting pathways that regulate lipid metabolism that can result in more effective treatments for patients suffering from these conditions.”
Read all the details of this work in the journal Science Advances.
Others involved in the study are Guang Lin, Zhongyuan Zuo, Yarong Li, Seul Kee Byeon, Akhilesh Pandey. They are affiliated with one or more of the following institutions: Baylor College of Medicine, Jan and Dan Duncan Neurological Research Institute, Texas Children’s Hospital, Mayo Clinic and Manipal Academy of Higher Education. The study was funded by the Huffington Foundation.