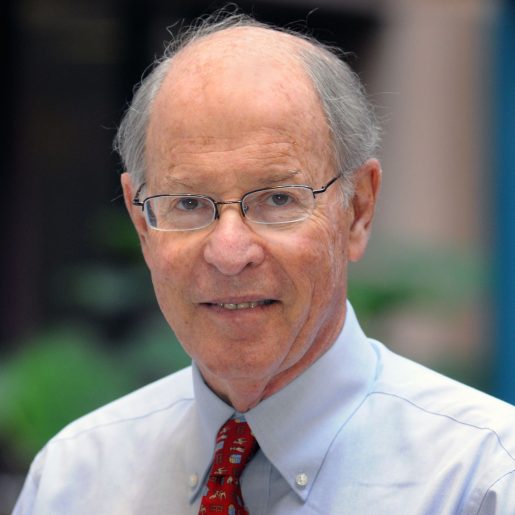
Understanding pneumonia: Interview with Dr. Daniel M. Musher
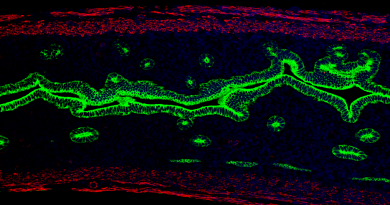
Pneumonia is an infection of the lungs that produces coughing, fever, chills, muscle aches and difficulty breathing. It has been recognized since ancient human history; however, despite medical and scientific advances, pneumonia remains one of the five most common causes of death worldwide.
To learn more about pneumonia, From the Labs sat with infectious diseases expert Dr. Daniel M. Musher, Distinguished Service Professor of Medicine and of Molecular Virology and Microbiology at Baylor College of Medicine and a member of the Infectious Diseases Section at the Michael E. DeBakey Veterans Administration Medical Center. He and Dr. Naomi J. Gadsby, a consultant clinical scientist in medical microbiology at the Royal Infirmary of Edinburgh, Scotland, and an Honorary Fellow of the University of Edinburgh, have written a review on this complex disease.
Published in Clinical Microbiology Reviews, a publication of the American Society for Microbiology, the review reveals the dynamic nature of our knowledge of pneumonia, which continues to evolve as new techniques enable identification of the microorganisms causing the disease, from already known microbes to new emerging organisms, as well as approaches to improve diagnosis and treatment.
FTL: Is it true that you have coauthored a total of 600 publications?
DMM: Yes. This review of the etiology or causes of pneumonia is No. 600. A couple more papers have already been accepted or are being submitted, as we speak.
FTL: What has driven your interest in studying pneumonia over the years?
DMM: Pneumonia is an important cause of death around the world, so by its very nature it’s worth studying. When I first went into medicine, it was taught that a single organism, pneumococcus, now called Streptococcus pneumoniae, which got its name because it causes pneumonia, was the overwhelmingly common cause of the disease. As a fellow in infectious diseases, I didn’t think that was true, but that was the consensus among experts.
FTL: How did you pursue your desire to better understand pneumonia?
DMM: I was always interested in the cause of the disease and in the methodology that would allow me to make a diagnosis. I find it both interesting and terribly important because you can reach totally different conclusions depending upon the care with which you apply your methods to your study.
FTL: What did your studies show you?
DMM: After very careful study I found results that are quite different from what was published. That made me go back and review the literature thoroughly. I found that through World War II most of the emphasis on the cause of pneumonia was placed on pneumococcus. But even then, physicians knew that viruses, especially influenza, were a big cause of the disease. A fair amount of those viral cases were complicated by bacteria, so pneumococcus was also a secondary cause. In the 1940s, researchers discovered that Mycoplasma pneumoniae also could cause pneumonia. By early 1970s, Chlamydia pneumoniae was found to usually cause the disease in young adults. You see, as I paint the picture, there are many different types of already known microorganisms that can cause pneumonia, but the textbooks kept saying that pneumococcus was the cause of all pneumonias.
FTL: What was your earliest major discovery?
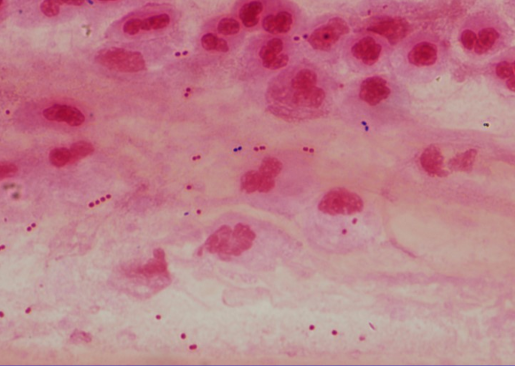
DMM: I showed that nontypeable Haemophilus influenzae is a prominent cause of pneumonia in adults, and the most recent studies show that it is as equally common as pneumococcus. I was seeing many patients presenting pneumonia symptoms. Some of them produced large amounts of sputum – a mixture of white blood cells, plasma and bacteria coughed up from the respiratory tract. I carefully prepared samples of sputum and studied them under the microscope. The sputum was filled with large numbers of bacteria that I quantified in culture and as a result identified abundant nontypeable H. influenzae (type B H. influenzae was discovered in the late 1800s during an influenza epidemic and thought to be its cause at the time, hence the name. We know now that a virus causes influenza).
Also, I showed that antibodies to Hemophilus emerge during these pneumonias, which proves that the organism is a cause of the infection. Studies from my lab and from others have shown that, in addition to Streptococcus pneumoniae, Haemophilus influenzae, Staphylococcus aureus, Moraxella catarrhalis, Enterobacteriaceae, Pseudomonas and normal respiratory flora also can cause pneumonia. Those findings came from simply being careful about clinical observation and the use of the laboratory. My whole career is based on that: observe clinically and use the lab to support the clinical observations, knowing the methodology and applying it.
FTL: What happened next?
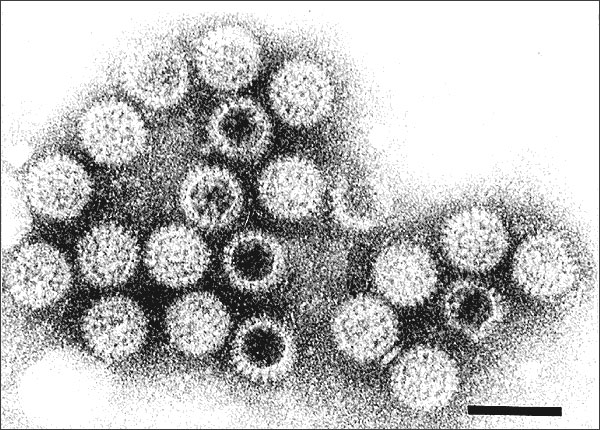
DDM: As new technologies emerged, such as PCR, it became possible to diagnose viral pneumonia, which can be caused by rhinovirus, respiratory syncytial virus (RSV) and other respiratory viruses. This has painted a more complex picture of pneumonia not only regarding its cause but also how to treat it.
FTL: Knowing that bacteria and/or viruses can be causing a person’s pneumonia, how would you go about reaching a diagnosis?
The big question in my field is, should everyone admitted to the hospital for pneumonia be treated with antibiotics?”
DMM: The answer is far from simple, but I would start with a good sputum sample and a nasal swab from the patient. The problem is that many patients do not readily provide good sputum samples, and physicians fail to encourage them to try. Without those, there really is no test currently available to tell whether a patient has bacterial or viral pneumonia. Analyzing the samples for the type of bacteria and viruses present would help determine the most probable cause of the infection. Unless it’s shown that there are not many bacteria in the sputum and the PCR demonstrates a respiratory virus, then the patient has to be treated with antibiotics, which only kill bacteria and do not affect viral growth.
FTL: What would be your advice to physicians seeing patients with pneumonia?
DMM: Go to a little extra trouble and tell the patient to take a few deep breaths in and out and cough up a good sputum sample that can be examined microscopically and sent to the lab. Until the result comes back from the lab, give an initial dose of antibiotics because you don’t want to wait too long.
FTL: What would you say to a patient with pneumonia?
DMM: I would encourage patients to work with their doctors to help find the cause of their pneumonia.
A patient can ask: “Well, doctor, what is the cause of my pneumonia?
Doctor: “We don’t really know.”
Patient: “Can you find out?”
Doctor: “Provide a good sputum sample that I can study to try find the cause.”
FTL: What else can doctors and patients do to better manage pneumonia?
DMM: It is always better to prevent it than to treat it. Getting the pneumococcal vaccine, as well as the flu, RSV and COVID vaccines, goes a long way in preventing and reducing symptoms of these serious respiratory diseases.