Is red meat intake linked to inflammation?

Inflammation is a risk factor for many chronic diseases, including cardiovascular disease (CVD), and the impact of diet on inflammation is an area of growing scientific interest. In particular, recommendations to limit red meat consumption are often based, in part, on old studies suggesting that red meat negatively affects inflammation – yet more recent studies have not supported this.
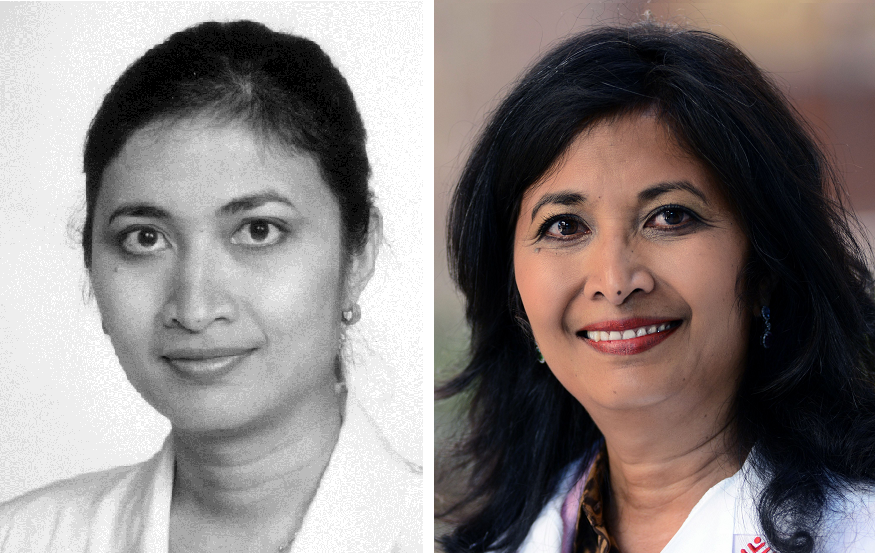
“The role of diet, including red meat, on inflammation and disease risk has not been adequately studied, which can lead to public health recommendations that are not based on strong evidence,” said Dr. Alexis Wood, associate professor of pediatrics – nutrition at the USDA/ARS Children’s Nutrition Research Center at Baylor College of Medicine and Texas Children’s Hospital. “Our team sought to take a closer look by using metabolite data in the blood, which can provide a more direct link between diet and health.”
Wood and her team analyzed cross-sectional data captured from approximately 4,000 older adults participating in the Multi-Ethnic Study of Atherosclerosis (MESA), and recently published their findings in The American Journal of Clinical Nutrition. Cross-sectional data is a useful source of evidence on how diet affects health; it uses data that is observed with free-living people, without attempting to influence their usual lifestyle. In this way, it may be easier to take results from such studies and apply them to non-research settings. In addition to assessing participants’ self-reported food intake and several biomarkers, researchers also measured an array of dietary intake metabolites in blood. Plasma metabolites can help capture the effects of dietary intake as food is processed, digested and absorbed.
Researchers found that when adjusted for body mass index (BMI), intake of unprocessed and processed red meat (beef, pork or lamb) was not directly associated with any markers of inflammation, suggesting that body weight, not red meat, may be the driver of increased systemic inflammation. Of particular interest was the lack of a link between red meat intake and C-reactive protein (CRP), the major inflammatory risk marker of chronic disease.
“Our analysis adds to the growing body of evidence that indicates the importance of measuring plasma markers, such as metabolites, to track diet and disease risk associations, versus relying on self-reported dietary intake alone,” Wood said. “Our analysis does not support previous observational research associations linking red meat intake and inflammation.”
Because observational studies cannot indicate cause and effect, randomized controlled trials (RCTs) where individuals are randomly assigned to consume a dietary factor of interest or not consume it, are needed as an additional line of evidence to adequately understand if red meat does not alter inflammation. Several RCTs have demonstrated that lean unprocessed beef can be enjoyed in heart-healthy dietary patterns.
“We have reached a stage where more studies are needed before we can make recommendations to limit red meat consumption for reducing inflammation if we want to base dietary recommendations on the most up-to-date evidence,” Wood said. “Red meat is popular, accessible and palatable – and its place in our diet has deep cultural roots. Given this, recommendations about reducing consumption should be supported by strong scientific evidence, which doesn’t yet exist.”
Other contributors to this work include Goncalo Graca, Meghana Gadgil, Mackenzie K. Senn, Matthew A. Allison, Ioanna Tzoulaki, Philip Greenland, Timothy Ebbels, Paul Elliott, Mark O. Goodarzi, Russell Tracy, Jerome I. Rotter and David Herrington.
The study was supported by the Beef Checkoff. Wood was supported, in part, by the USDA/ARS (Cooperative Agreement 58-3092-5-001). Mark Goodarzi was supported by the Eris M. Field Chair in Diabetes Research. Jerome Rotter was supported, in part, by the National Institutes of Health grants from the National Institute of Diabetes and Digestive and Kidney Disease (DK063491), from the National Center for Advancing Translational Sciences (UL1TR001881), the CHARGE Consortium, and the National Heart, Lung, and Blood Institute (NHLBI; R01HL105756).
By Homa Warren