Molecular profiling identifies new high-risk subtype of pediatric liver cancer
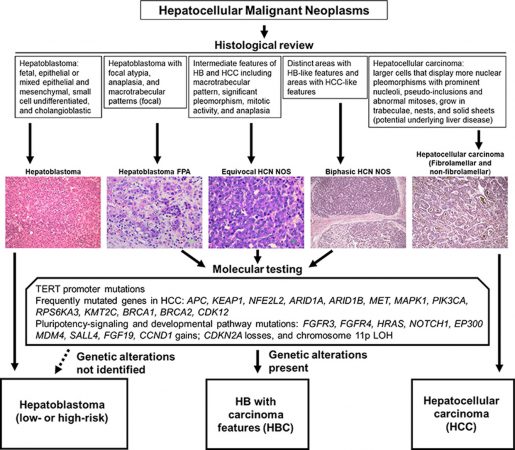
Until recently, nearly all pediatric liver cancers were classified as either hepatoblastoma or hepatocellular carcinoma. However, pediatric pathologists observed that some liver tumors have histological features that do not easily fit neither of these two carcinoma models. These cancers are less likely to respond to chemotherapy and patient outcomes are poor.
First author Dr. Pavel Sumazin, associate professor of pediatrics at Baylor College of Medicine and Texas Children’s Cancer and Hematology Center, and his colleagues looked to better characterize this high-risk cancer.

The researchers examined the molecular profiles of the tumors, including genetic alterations and gene expression profiles. They found that these profiles do not fit into the hepatoblastoma (HB) or hepatocellular carcinoma (HCC) molecular categories. Instead, these tumors exhibited recurring molecular features that have been observed in both HBs and HCCs. They designated these tumors as hepatoblastomas with hepatocellular carcinoma features (HBCs).

The team also examined HBC treatments and outcomes and found that they tended to be more resistant to standard chemotherapy and have poor outcomes when not treated with more aggressive surgical approaches, including transplantation. Based on their findings, the researchers proposed a diagnostic algorithm to stratify HBCs and guide specialized treatment.
“Our findings highlight the importance of molecular testing to accurately classify these tumors to optimize treatment recommendations at the time of initial diagnosis,” said Dr. Dolores López-Terrada, corresponding author of the paper, professor of pathology, immunology and pediatrics at Baylor and chief of the division of genomic medicine at Texas Children’s.
Our analysis suggested that children with HBCs may benefit from treatment strategies that differ from the guidelines for patients with hepatoblastoma and hepatocellular carcinoma.”
Find all the details of this study in the Journal of Hepatology.
Sumazin and López-Terrada both are members of the Dan L Duncan Comprehensive Cancer Center at Baylor. Other authors from Baylor and Texas Children’s include Tricia L. Peters, Stephen F. Sarabia, Hyunjae R. Kim, Martin Urbicain, Emporia Faith Hollingsworth, Karla R. Alvarez, Cintia R. Perez, Mohammad Javad Najaf Panah, Jessica L. Epps, Kathy Scorsone, Barry Zorman, Sarah E. Woodfield, John A. Goss, Sanjeev A. Vasudevan, Andras Heczey, Angshumoy Roy, Kevin E. Fisher, Kalyani R. Patel and Milton J. Finegold.
Howard Katzenstein, Allison F. O’Neill, Rebecka Meyers, Greg Tiao, Jim Geller, Sarangarajan Ranganathan, Arun A. Rangaswami, all members of the Children’s Oncology Group Liver Tumor Committee, as well as Rita Alaggio and Alice Pozza also contributed. They are from the following institutions: Wolfson Children’s Hospital, Dana-Farber Cancer Institute, Boston Children’s Hospital, Harvard Medical School, Primary Children’s Hospital, Cincinnati Children’s Hospital Medical Center, University of California San Francisco and Bambino Gesù Children’s Hospital.
This work was funded by the Cancer Prevention and Research Institute of Texas (RP180674), the European Union’s Horizon 2020 (826121), the Schindler Foundation and the National Cancer Institute (R21CA223140).
By Molly Chiu