CAR NKT cells, a promising step forward in the treatment of solid tumors
Solid tumors present a number of characteristics that have challenged the effectiveness of treatments. For instance, while immunotherapies involving chimeric antigen receptor (CAR)-modified immune T cells have proven to be effective in treating non-solid tumors such as certain types of leukemia and lymphoma, their effectiveness in solid tumors has been more limited.
Researchers at Baylor College of Medicine and the University of North Carolina at Chapel Hill have taken a step forward in the treatment of solid tumors. The team genetically modified human Natural Killer T (NKT) cells with a chimeric antigen receptor that enables the cells to specifically recognize and attack neuroblastoma, a form of childhood cancer. Expressed with the CAR is interleukin-15 (IL-15), a natural protein that supports NKT cell survival.
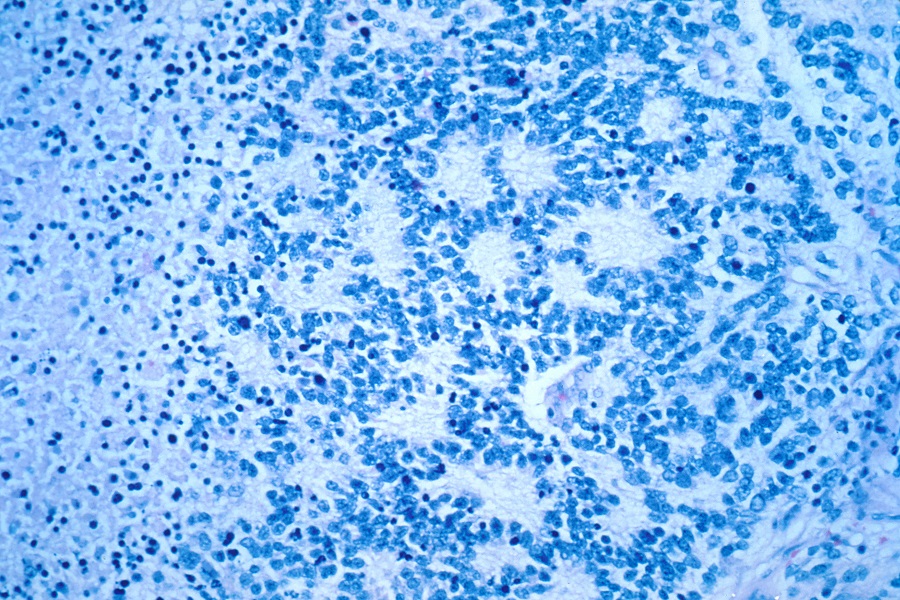
NKT cells are a type of immune cells known for their potent anti-cancer properties in murine tumor models. In the current study, appearing in Nature Medicine, the researchers present interim results from an ongoing clinical trial showing that modified human NKT cells are safe, localize to tumors, and, in one of three patients, induced an objective response with regression of bone metastatic lesions.
Enhancing the tumor-fighting capabilities of NKT cells
Preclinical studies have shown that NKT cells offer a novel approach that may enhance CAR-directed cancer immunotherapy.

“In addition to being able to effectively combat tumors in mouse models, the presence of NKT cells within solid tumors is associated with favorable outcomes in cancer patients,” said co-corresponding author Dr. Leonid Metelitsa, professor of pediatric oncology at Baylor and Texas Children’s Hospital and member of Baylor’s Dan L Duncan Comprehensive Cancer Center.
Previous work has shown that NKT cells have a spectrum of anti-tumor activities. For instance, these cells migrate to tumor sites where they kill tumor-associated macrophages, a type of immune cell that can promote tumor growth and metastasis. Moreover, NKT cell activation indirectly promotes an anti-tumor response mediated by two other types of immune cells, NK and T cells.
“We think that NKT cells have substantial potential to serve as valuable contributors to the fight against cancer,” said co-corresponding and first author Dr. Andras Heczey, assistant professor of pediatric oncology at Baylor and Texas Children’s and member of the Dan L Duncan Comprehensive Cancer Center.
For the last 10 years, we have been focused on enhancing these cells’ tumor-fighting abilities with the ultimate goal of bringing them to the clinic.”
Preparing NKT for clinical trials
The journey to develop NKT cells into a form of immunotherapy involved finding solutions for a number of challenges. For example, NKT cells represent a low percentage of the cells in the blood, so Metelitsa, Heczey and their colleagues developed methods to grow NKT cell populations to clinical scale with high purity.
Although NKT cells can combat tumors in several ways, they all seem to be indirect. “So, working with Dr. Gianpietro Dotti at UNC, we gave NKT cells a tool – the CAR – that enables them to attack tumors directly,” Metelitsa said. “We also equipped them with IL-15, an additional tool to help them survive in the patient while they fight the tumor.”
“The field of CAR cellular immunotherapy for cancer has been focused to date primarily on the manipulation of T lymphocytes,” said Dotti, professor and director of cancer cellular immunotherapy at UNC Lindberger Comprehensive Cancer Center. “Based on previous clinical evidence that NKT infiltration within the tumor correlates with favorable clinical outcomes, we decided to leverage this intrinsic property of NKTs and to arm them with an additional bullet – the so-called CAR – to further potentiate their capacity to destroy the tumor.”
With all these innovations in hand, the researchers moved on to test CAR NKT cells in patients with neuroblastoma in a clinical trial.
Clinical results
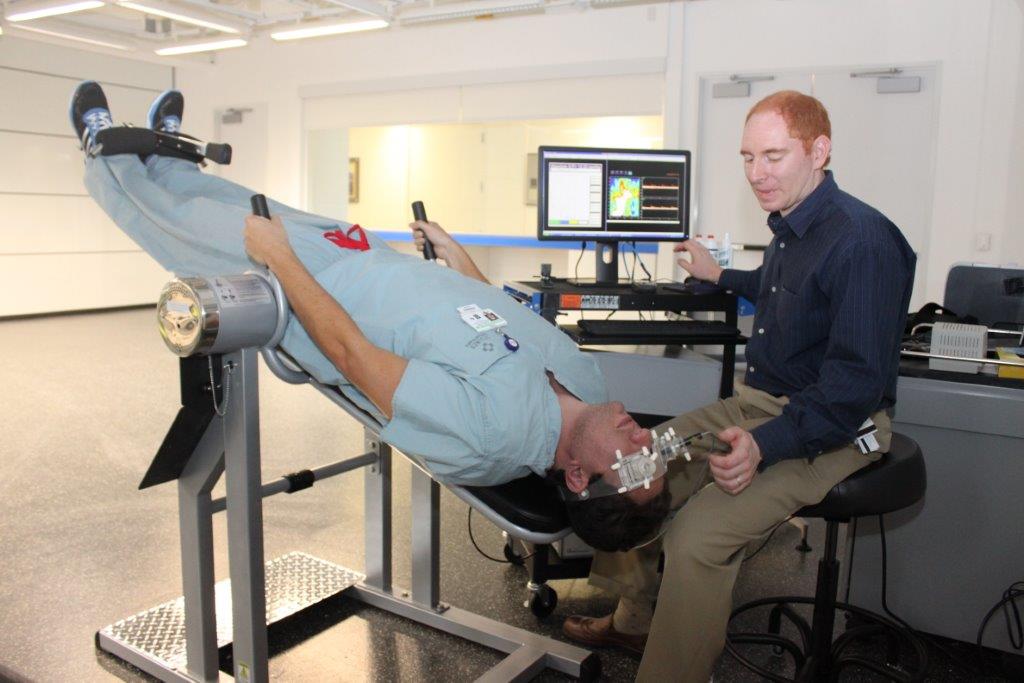
The clinical trial is ongoing, and results from the first three patients with heavily pre-treated, relapsed/refractory metastatic neuroblastoma are presented in this study. The patients were treated with CAR NKT cells, engineered from the patient’s own white blood cells at the Center for Cell and Gene Therapy at Baylor and Texas Children’s. Researchers engineered 95 percent pure NKT cells, a portion of which was armed with CAR-IL15.
Our initial results show that NKT cells can be expanded to clinical scale with high purity, genetically engineered to express a CAR and IL15, and used to safely treat patients with advanced neuroblastoma,” Metelitsa said.
“In addition, we found that CAR-IL15 NKT cells can be detected in the peripheral blood, where they expand after infusion, traffic to bone metastases and the bone marrow, and exert anti–tumor activity,” Heczey said. “We observed an objective response, elimination of at least 50 percent of metastases, in one of the patients.”

Dr. Antonio Montalbano and other co-authors from Immunai, a company specializing in single-cell technologies and AI approaches for immunology, applied its state-of-the-art technology platform that allows for the analysis of all genes at the single-cell level in the CAR-NKT patient products. These analyses revealed new information about the heterogeneity of human NKT cells and molecular details of their therapeutic modifications. The researchers discovered nine subsets of NKT cells, and that the CAR receptor seemed to go preferentially to one set identified as cluster 3. Further studies will help understand the implications of these findings.
“Our study shows that it is possible to employ immune cells with natural anti-tumor capabilities and enhance their tumor fighting power with designer synthetic receptors, opening the possibility of applying this strategy to combat hard-to-treat solid tumors,” Metelitsa said.
“By leveraging Immunai’s end-to-end platform of artificial intelligence and computational analysis, we were able to zero in on CAR engineered NKT cells from the patients at the single-cell level. The findings from this study are critical toward developing more precise and effective therapies for cancer patients,” said Montalbano, genomics technologies lead at Immunai. “We’re looking forward to continuing our research with Baylor with the goal of advancing therapeutic discoveries, accelerating drug development and improving patient outcomes.”
The NKT platform developed in this research at Baylor has been licensed to Kuur Therapeutics to advance clinical development.
“The Baylor-Kuur Therapeutics relationship is generating exactly the type of outcomes that we had envisioned at the outset,” said Shawn Davis, vice president and chief ventures officer at Baylor. “The modified NKT platform developed in the Metelitsa laboratory is differentiated from other cell therapy platforms, offering novel routes for the treatment of cancers that have posed challenges for immunotherapeutic approaches. The encouraging findings announced today support the potential of NKT platform to provide promising alternatives, particularly for the treatment of solid tumors.”
Other contributors to this work include Amy N. Courtney, Simon Robinson, Ka Liu, Mingmei Li, Nisha Ghatwai, Olga Dakhova, Bin Liu, Tali Raveh-Sadka, Cynthia N. Chauvin-Fleurence,Xin Xu, Ho Ngai, Erica J. Di Pierro and Barbara Savoldo. The authors are affiliated with one or more of the following institutions: Baylor College of Medicine, Texas Children’s Hospital, Immunai Inc. and the University of North Carolina at Chapel Hill.
This work was supported by grants/contracts from Alex’s Lemonade Stand Foundation for Childhood Cancer, Kuur Therapeutics, American Cancer Society, Cookies for Kids’ Cancer Foundation and the Cancer Prevention and Research Institute of Texas (BCM Comprehensive Cancer Center Training Program, RP160283).