Becoming metastatic: how FOXA1 triggers metastatic behavior in breast cancer
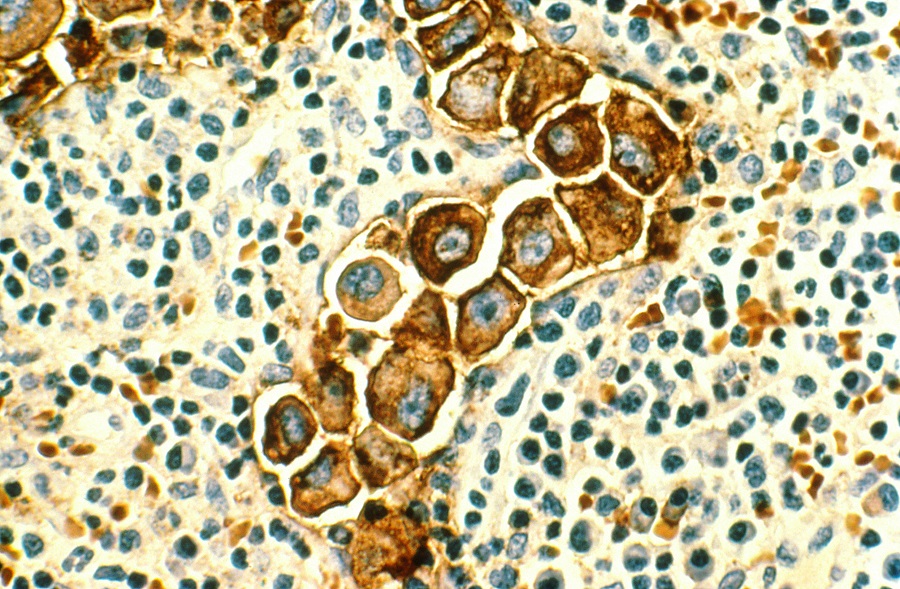
About 75 percent of breast cancers have estrogen receptors, hence they are called estrogen receptor positive (ER+). Original ER+ breast cancer cells depend on estrogen to grow, and therapies that make estrogen unavailable to cells, called hormone therapies, can result in long-term remission in some patients. Tamoxifen, one of several types of hormone therapy, works by binding to and blocking the estrogen receptor on cancer cells.
However, most patients with metastatic disease, including those whose tumors responded initially to hormone therapy, eventually relapse and die due to the tumors’ acquired resistance to hormone therapy.
In her laboratory at Baylor College of Medicine, Dr. Rachel Schiff and her colleagues, together with collaborators at Harvard Medical School, have unveiled a novel mechanism that helps explain how endocrine-resistant breast cancer acquires metastatic behavior, opening the possibility of new therapeutic strategies.

“In previous work, we discovered that tumor cells resistant to hormone therapies make more FOXA1 than susceptible cells, and this abundance of FOXA1 plays an active role in conferring resistance to the therapy,” said Schiff, associate professor of medicine and the Lester and Sue Smith Breast Center at Baylor and co-corresponding author of this work.
In the current study, the researchers took a genome-wide approach to dig deeper into how FOXA1 accomplishes the complex task of triggering metastatic behavior.
Changing the program triggers metastatic behavior
“Working with breast cancer cell lines in the laboratory, we discovered that FOXA1 reprograms endocrine therapy-resistant breast cancer cells by turning on certain genes that were turned off before and turning off other genes. The new gene expression program mimics an early embryonic developmental program that endows cancer cells with new capabilities, such as being able to migrate to other tissues and invade them aggressively, hallmarks of metastatic behavior,” said first and co-corresponding author Dr. Xiaoyong Fu, assistant professor of molecular and cellular biology and part of the Lester and Sue Smith Breast Center at Baylor.
The researchers also discovered that FOXA1 does not act alone. Along with other factors, it activates a large number of enhancers that work together to synchronize genome-wide cell reprogramming. HIF-2a is the top enhancer working with FOXA1 mediating the activation of pro-metastatic gene sets and pathways associated with poor clinical outcome.
Importantly, the researchers showed in laboratory cell experiments that an inhibitor of HIF-2a, currently under clinical development for treatment of advanced renal cell carcinoma and recurrent glioblastoma, reduced migration and invasion of endocrine-resistant breast cancer cells expressing high FOXA1 activity.
“In collaboration with our colleagues from Harvard Medical School, we explored the possibility of transferring these findings to the clinic. We analyzed clinical metastatic breast cancer datasets and discovered reprogramming events that were similar to those found in our endocrine-resistant breast cancer cell models,” said Schiff, who also is a member of the Dan L Duncan Comprehensive Cancer Center at Baylor. “These findings support investigating whether inhibiting HIF-2a or other enhancer that controls the expression of many genes in endocrine therapy-resistant breast cancer could be translated into effective therapeutic strategies.”
Taken together, these discoveries reveal details of the intricate mechanism FOXA1 triggers to induce metastatic behavior in endocrine-resistant breast cancer, which other reports have suggested also is present in other types of cancer, such as prostate and pancreatic cancer.
Interested in all the details of this study? Find them in the Proceedings of the National Academy of Sciences.
Find the complete list of contributors to this work, their affiliations and financial support for this project in this link.