Connecting seizures, neurogenesis and cognitive functions in Alzheimer’s disease
Whether the normal adult human brain produces new neurons, much less those with Alzheimer’s disease, is a controversial topic in the field. While some groups present evidence supporting a decrease in neurogenesis, others claim that it increases or that there is no change. Working with mouse models of the disease, the lab of Dr. Jeannie Chin at Baylor College of Medicine has identified a mechanism that the researchers propose may integrate all of these apparently contradicting findings.
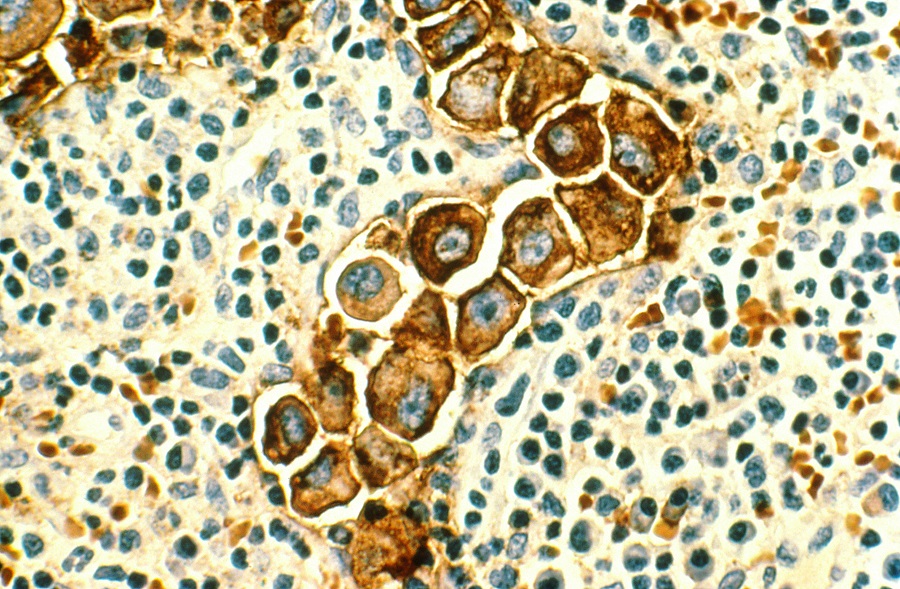
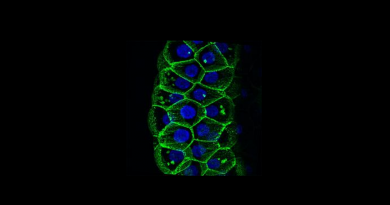
Scientists have found that in normal mice neurogenesis occurs throughout life and decreases as the animals age. Neurogenesis is a multistep process that begins with the proliferation of neural stem cells, continues with the production of intermediary cells such as progenitor cells, and ends with new neurons being born.
Findings from Chin’s collaborators demonstrated that the pool of neural stem cells in the brain is finite. After a certain number of cell divisions, a neural stem cell stops being a stem cell, and is not replaced. Consequently, throughout the life of normal mice, the number of neural stem cells progressively decreases.
Silent seizures and adult neurogenesis
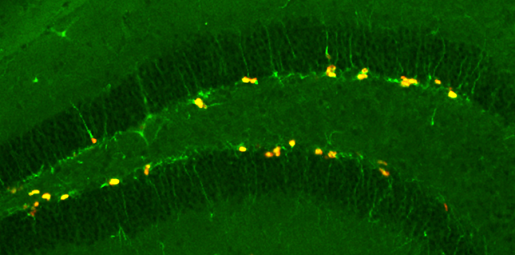
“In this study, we compared the process of neurogenesis in normal mice with that in our mouse model of Alzheimer’s disease, and found that the processes are similar but, when seizures occur in mice with the disease, neurogenesis is acutely stimulated,” said first author Chia-Hsuan Fu, neuroscience graduate student in the Chin lab.
The researchers observed that early in the disease when seizures begin, there is an increase in neurogenesis as neural stem cells are stimulated to divide. As the disease progresses and seizures recur stimulating more neural stem cells, the cell pool is depleted faster than in animals without the disease, and neurogenesis decreases. Later in the disease, when the pool of cells is exhausted, there is very little neurogenesis.

“Although our study was conducted in mice, we suggest that the level of neurogenesis in a human brain with Alzheimer’s disease may similarly depend on the stage of the disease, being higher at very early stages and then declining more rapidly than normal as disease continues,” said Fu. “The level of neurogenesis would depend on when during the disease the samples were taken. These findings may explain the seemingly contradictory findings about whether and how neurogenesis is affected in Alzheimer’s disease.”
Chin and her colleagues also speculated that the mechanism they discovered may also help explain controversial studies regarding whether adult neurogenesis, which has primarily been studied in rodents, occurs at all in humans. “Depending on the medical history of the patients from whom the brain samples were obtained, they might have high, low or even nonexistent levels of neurogenesis at the time of death,” said Chin, who is associate professor of neuroscience at Baylor.
A potential improvement
Interestingly, when the researchers treated their mouse model with anti-seizure drugs they normalized the dynamics of neurogenesis. Further, animals treated with anti-seizure drugs improved their performance in a spatial discrimination task when compared with non-treated mice.
Taken together, the findings suggest that the seizures are deeply connected to the alterations in neurogenesis and cognitive functions both in Alzheimer’s disease and epilepsy.
They also were expecting that accumulation of amyloid-beta in the brain, a major hallmark of the disease, would affect neurogenesis as suggested by experiments in the labs of other groups. However, the observations of Chin and her colleagues rather indicate that the effect of seizures on neurogenesis seems to be larger than that of amyloid-beta accumulation.
The finding that anti-seizure medications can normalize the process of neurogenesis in an animal model of the disease suggests that it also might be possible to do so in human patients.
“However,” Chin remarks, “more work is needed and caution is necessary because the medication would have to be administered early in the disease, just as seizures are beginning to occur.”
Find all the details of this work in the journal Cell Reports.
Other contributors to this work include Daniel Maxim Iascone, Iraklis Petrof, Anupam Hazra, Xiaohong Zhang, Mark S. Pyfer, Umberto Tosi, Brian F. Corbett, Jingli Cai, Jason Lee, Jin Park, Lorraine Iacovitti, Helen E. Scharfman and Grigori Enikolopov. The authors are affiliated with one or more of the following institutions: Baylor College of Medicine, Thomas Jefferson University, New York University Langone Medical Center and Stony Brook University.
This work was supported by the National Institutes of Health (grants NS086965, NS085171, NS075839, NS086965, AG040209 and NS086965) and the New York State Office of Mental Health.