USP15 could be a target in ovarian cancer scientists have been looking for
Ovarian cancer is currently treated with surgery and chemotherapy. Chemotherapy for ovarian cancer is based on drugs that act on any cell that is rapidly dividing, healthy or malignant, which has significant side effects.
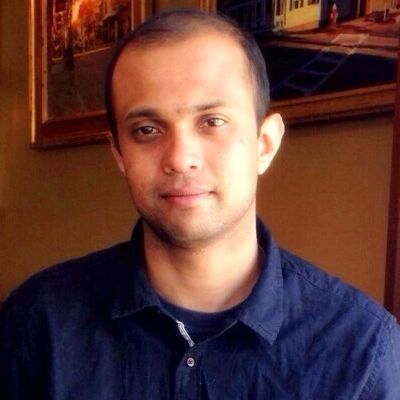
“If we are able to develop treatments that target only cancer cells, then we might be able to minimize side effects,” Dr. Achuth Padmanabhan, instructor of molecular and cell biology at Baylor College of Medicine.
Researchers have revealed that mutant p53 proteins might be the target scientists have been looking for. More than 96 percent of high-grade serous ovarian carcinomas, the most lethal and common form of ovarian cancer, have mutations in the p53 gene. These mutations have been shown to play key roles in the production of tumors and in the development of drug resistance. Normal p53 protein is known for playing a tumor suppressor role. In contrast, the mutation studied by Padmanabhan and his colleagues – p53-R175H – can promote tumor growth.
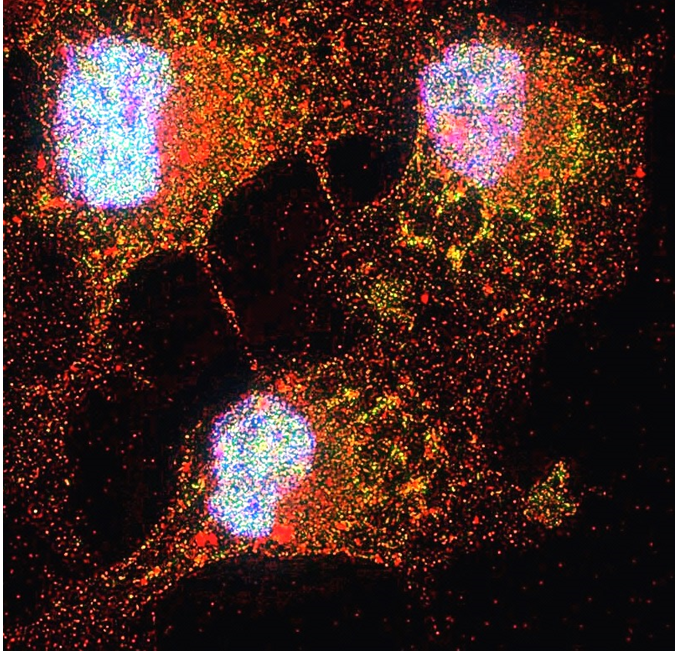
“Normal p53 is rapidly broken down inside most healthy cells, but p53 mutants such as p53-R175H, are not. They form very stable protein clusters inside cells that promote cancer and induce drug resistance,” Padmanabhan said. “Researchers have discovered that if we remove the mutant p53 forms from cancer cells, the cells will enter a path toward cell death and become more sensitive to chemotherapy. This is very valuable from the clinical point of view.”
These findings have prompted Padmanabhan and his colleagues and other researchers to find ways to reduce the levels of p53-R175H inside cancer cells to promote their own destruction.
A potential new way to fight ovarian cancer
“The question has been how to selectively eliminate p53-R175H clusters. We do not want to affect the normal p53 proteins because this also can lead to cancer. Our goal is to find ways to reduce the levels of mutant p53-R175H only,” Padmanabhan said. “We did not know how to do it until we discovered a unique pathway than can regulate the mutant, but not normal p53. Once we identify the specific pathways, we can design drugs to manipulate them.”

When Padmanabhan began working in the lab of Dr. JoAnne Richards at Baylor College of Medicine, they were testing a small molecule called MCB613, for its ability to treat ovarian cancer in a mouse model of the disease. In those experiments, Padmanabhan observed that in cells treated with MCB613 the levels of mutant p53 protein rapidly decreased.
“This was interesting because it told me that the drug was doing something unique to this mutant, but not to the other forms of p53,” Padmanabhan said. “In this work, we tried to understand how treatment with MCB613 resulted in reduced levels of p53-R175H in ovarian cancer cells.”
The researchers found that MCB613 does not decrease the levels of mutant p53-R175H protein directly. It reduces the levels of another protein called USP15 that removes a specific tag from the p53 mutant that targets it to undergo degradation inside cells.
“Having fewer molecules of USP15, results in more mutant p53-R175H protein tagged for degradation in the cell,” Padmanabhan said. “As a result, the balance tips toward elimination of mutant p53-R175H proteins, which results in more cancer cell death. We also discovered that mutant p53-R175H is destroyed in the lysosome system of the cell, as opposed to normal p53, which is broken down by another protein-degradation system within the cells called the proteasome.”
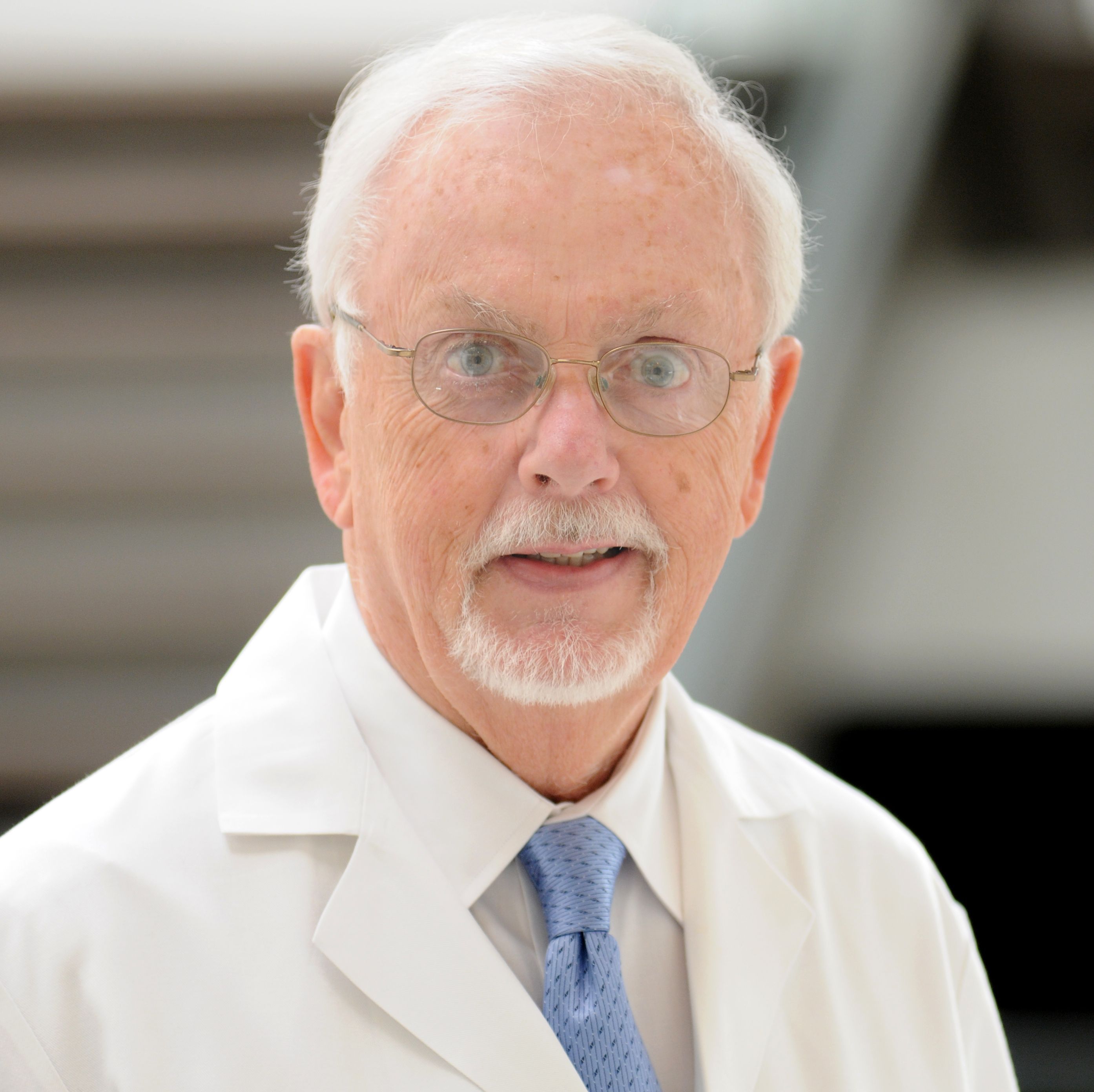
“Our findings offer a new opportunity for regulating mutant p53-R175H by developing drugs that inhibit USP15,” said Richards, professor of molecular and cellular biology and member of the Dan L Duncan Comprehensive Cancer Center at Baylor College of Medicine.
A possible future scenario in the clinic could be to use DNA analysis to determine whether this p53 mutation is present in a patient’s tumor. If so, then we may use our approach to treat it or combine it with other anticancer drugs and take advantage of the fact that treatment with inhibitors of USP15 results in the cancer cells becoming more susceptible to chemotherapy,” Padmanabhan said.
The researchers also found that mutant p53-R175H is more sensitive to ovarian steroids, so they are looking at how ovarian steroids affect ovarian cancer progression.
“We are combining ways of regulating steroid receptor and coactivator action, as well as p53,” said co-author Dr. Bert O’Malley, chair and professor of molecular and cellular biology, Thomas C. Thompson Chair in Cell Biology and associate director of basic research in the Dan L Duncan Comprehensive Cancer Center. “Maybe by manipulating both of those pathways we may have a better chance of regulating cancer growth.”
Find all the details about this work in the journal Nature Communications.
Other contributors of this work include Nicholes Candelaria, Kwong-Kwok Wong, Bryan Nikolai and David M Lonard.
This work was supported by NIH grant NIH-CA-181808 to JSR. Imaging was supported by the Integrated Microscopy Core at BCM with funding from NIH (DK56338, and CA125123), CPRIT (RP150578), the Dan L. Duncan Comprehensive Cancer Center and the John S. Dunn Gulf Coast Consortium for Chemical Genomics.


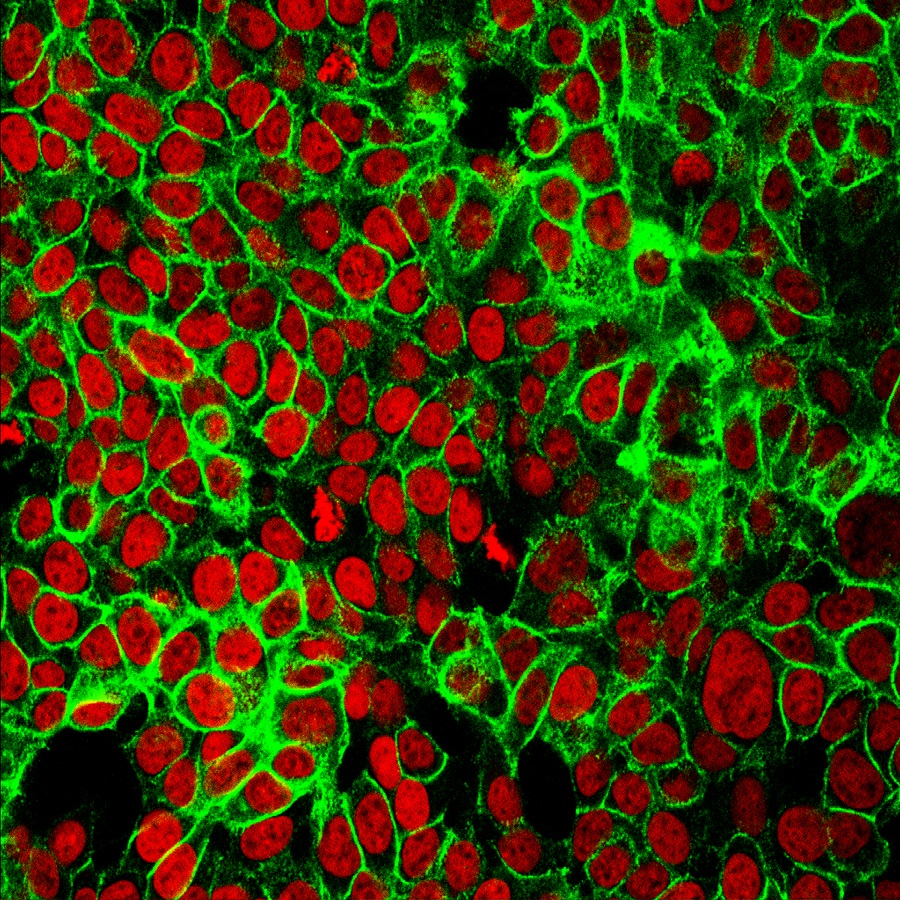
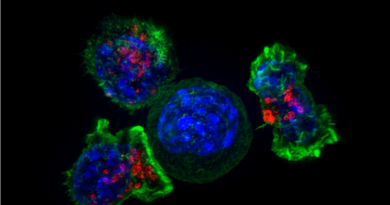
Pingback: Image of the Month: ovarian cancer cells