Not committed to fail: novel approach improves heart failure outcomes in animal model


In 2020, heart failure affected about 6.5 million people in the U.S. and 23 million around the world. Despite recent advances, the five-year survival rate remains approximately 50%, indicating an urgent need for a novel perspective for treating this condition.
“Current treatments do not directly treat the cells damaged in heart failure. Our goal was to do just that, to correct the metabolic changes in diseased heart cells that play a role in the organ’s failure,” said co-corresponding author Dr. Lilei Zhang, associate professor of molecular and human genetics and of integrative physiology at Baylor College of Medicine.
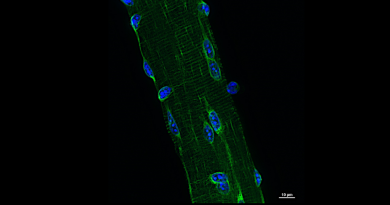
One of the hallmarks of heart failure is that diseased cells express a different set of genes than those expressed by healthy heart cells.
“We see changes in gene expression that alter cardiac fuel metabolism and mitochondrial function,” Zhang said. The mitochondria are structures within cells that generate the energy cells need to function.
The goal of the researchers was to change the gene expression in the diseased heart so it becomes healthier.
Previous work had shown that estrogen-related receptors (ERRs), specifically ERR-alpha and ERR-gamma, in mouse heart cells are important for cardiac metabolism; they are involved in regulating the use of cellular fuel, such as fatty acids and glucose, as well as mitochondrial function that generates energy, functions that are altered in heart failure.
In addition, analysis of human heart muscle showed that the expression of a set of genes regulated by ERR-alpha was collectively reduced in failing human hearts. These findings suggested that promoting the activity of ERRs could potentially improve cardiac metabolism and consequently stop or reverse the progression of heart failure. The obstacle was the long belief in the field that it was not possible to target ERR-alpha.
Developing the right tools
Zhang joined forces with Dr. Thomas Burris, director and chair of the Department of Pharmacodynamics at the University of Florida, an expert in designing drugs to target receptors such as ERRs.
The team is the first to develop two structurally distinct ERR agonists or drugs named SLU-PP-332 and SLU-PP-915, that interact with ERRs and mediate the desired changes in metabolic genes. This new evidence supports revising the idea that it is not possible to target these receptors.
Encouraging results
“We tested the agonists in an animal model that mimics how chronic high blood pressure leads to heart failure in people,” Zhang said.
In the model, called pressure overload model, the heart must work extra hard to keep the blood flowing. Sustained extra effort on the heart’s part leads to structural changes, the heart muscle becomes bigger (hypertrophy) to work against the pressure and then it eventually fails. This process is typical of many people with heart failure.
The results with the agonists were very encouraging. The animals treated with the ERR agonists, although they had enlarged hearts working against increased pressure, their hearts did not fail.”
“On the other hand, the enlarged hearts of the animals that did not receive the ERR agonists did fail, as expected,” Zhang said. “The agonists boosted the metabolism to match the hypertrophy providing enough energy for the heart to sustain the extra activity and not fail.”
These results are important because the current understanding in the field is that once hypertrophy is established, the heart is committed to fail.
Our findings in the animal model show that a hypertrophic heart is not necessarily committed to failure. If we improve metabolic functions, we reduce the risk of it failing,” Zhang said.
“These findings have encouraged us to pursue clinical trials in the future to determine the value of ERR agonists to extend the survival in people with this condition, especially people with existing hypertrophy of the heart.”
Learn all the details of this study in the journal Circulation.
Weiyi Xu, Cyrielle Billon, Hui Li, Andrea Wilderman, Lei Qi, Andrea Graves, Jernie Rae Dela Cruz Rideb, Yuanbiao Zhao, Matthew Hayes, Keyang Yu, McKenna Losby, Carissa S. Hampton, Christiana M. Adeyemi, Seok Jae Hong, Eleni Nasiotis, Chen Fu, Tae Gyu Oh, Weiwei Fan, Michael Downes, Ryan D. Welch, Ronald M. Evans, Aleksandar Milosavljevic, John K. Walker, Brian C. Jensen and Liming Pei also contributed to this work. The authors are affiliated with one or more of the following institutions: Baylor College of Medicine, University of Health Sciences and Pharmacy in St. Louis, Washington University School of Medicine in St .Louis, University of North Carolina, University Hospitals Cleveland Medical Center, Salk Institute for Biological Studies, Howard Hughes Medical Institute, Blackburn College, Children’s Hospital of Philadelphia and University of Pennsylvania.
This work was supported by National Institutes of Health grants R01 HL143067, R01 HL150589, R21 HL165270, R43 HL160236 and DK111495.
Follow From the Labs on X @BCMFromtheLabs and Instagram!