Is it fair to be on multiple waitlists for an organ transplant?
Transplantation is a crucial treatment option for various end-organ diseases, and in the U.S., the demand for organ transplants outpaces the supply. One hotly debated issue concerns whether the existing policy that allows patients to be listed for an organ transplant across multiple centers is ethical. While the policy has been in place since 1987, it has been contentious. Many argue that it provides an unfair advantage to certain patients and perpetuates socioeconomic disparities in access to transplantation.
The U.S. transplant community has transplanted more than 1 million organs, the highest number worldwide, but the waitlist for transplants continues to grow. How do we allocate a limited resource to an ever-increasing group of patients? The Ethics Committee of the United Network for Organ Sharing (of which I am a part) recently evaluated the multiple-listing policy and recommended in a white paper that it should be “retained as an option only for patients who are exceptionally difficult to match.”
In this white paper, we present a history of multiple listing and an analysis of the ethical principles involved in its implementation as well as a review of the relevant data about its use.
Multiple listing is a contentious issue because it may give patients with greater resources an unfair advantage over those with less access. Patients who are listed at multiple centers for kidney transplantation could receive a kidney transplant nearly two years earlier than those who are listed at only one center. Moreover, patients who are listed at multiple centers for liver transplantation have a lower MELD score (a metric used to determine the severity of illness and one’s place on the waitlist) than those who are listed at only one center.
The available data presented in this white paper shows that education and insurance status contribute to the likelihood of receiving a transplant through multiple listings. “Patients with less than a high school education are 50% less likely to be multiple listed for a kidney or liver transplant, while those with a post-college graduate degree are 60% more likely to be multiple listed for liver and kidney transplant. Patients with Medicaid are at least three times less likely to be multiple listed than those with private insurance for kidney and liver transplant.” These findings suggest that multiple listings can exacerbate socioeconomic inequities in transplant access and availability.
While only 6% of all eligible patients are listed at multiple centers, this percentage amounts to thousands of transplant patients. The organ donation and transplant community has been under intense scrutiny to maximize the utility of the organs available and equity in the allocation of care. For example, the National Academy of Sciences, Engineering and Medicine called for equity improvements in the U.S. organ allocation and transplant system within the next five years and published their recommendations in a profound report titled Realizing the Promise of Equity in the Organ Transplantation System.
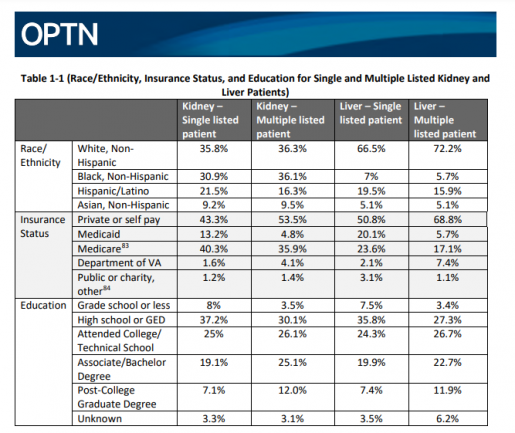
and education; taken from https://optn.transplant.hrsa.gov/media/l5odohtm/ethical-evaluation_multiple-listing_white-paper_ethics_pc-winter-2023.pdf
The report outlines that there is an opportunity to refocus the organ transplantation system and calls for expanding oversight and data collection, aligning providers with the goal of equity, shared decision-making with patients and public education and elevating voices of those facing disparities. Their recommendations align with those outlined in CFR 42 Subpart K §121.4 of the U.S. Common Rule, which federally regulates the equitable allocation of cadaveric organs in the U.S.
One argument against eliminating the policy of multiple listing is that it would infringe on the ethics of care and autonomy. Potential solutions include financial assistance to improve access, though this seems like a flawed argument. If we say that every single patient is given the option to multiply list and they do, then we are in the same situation as if there was no multiple listing at all. So why does this policy exist in the first place? We as an organization constantly work toward creating greater justice in a biased system. Why continue a practice that further exacerbates a known inequity? It is important to acknowledge that the ethics of allocation systems support our policies to determine the fair allocation of scarce resources, which in this case is a public enterprise.
This policy exacerbates socioeconomic disparities as it currently stands. Efforts are being made to improve equity in the public enterprise of organ allocation and continued scrutiny of the multiple-listing policy is needed to ensure that it aligns with the ethical principles that guide our policies, promoting equity and fairness in the allocation of organs while still accommodating those with medical need/exception.
As a member of society who may be impacted by organ donation and transplantation in some way, I invite you to read the white paper on multiple listing here, and please analyze and comment on the analysis here by March 15 to contribute to the conversation on how we can best allocate organs for patients in need.
– By Dr. N. Thao Galvan, associate professor of surgery – abdominal transplantation and Health Policy Scholar in the Center for Medical Ethics and Health Policy at Baylor College of Medicine