CSI-style scientific investigation finds answers for Mesoamerican Nephropathy
Mesoamerican Nephropathy (MeN) has puzzled physicians and scientists for more than 20 years. MeN refers to an epidemic of chronic kidney disease (CKD) of unknown origin that has severely affected specific coastal communities along Central America’s Pacific coastline from Mexico to Panama leading to more than 50,000 deaths.
The condition is puzzling because, unlike traditional forms of CKD, MeN affects healthy young working-age individuals who do not have other traditional risk factors for kidney disease, such as diabetes or hypertension.

“A few years back, based on my reputation of investigating many new outbreaks and my laboratory’s expertise in studying tropical medicine and infectious diseases among vulnerable populations, we were called to investigate the possible causes of this horrific epidemic,” said Dr. Kristy Murray, professor of pediatrics, immunology and microbiology at Baylor College of Medicine and Texas Children’s Hospital.
Murray initially received her outbreak experience twenty years ago at the CDC as part of the elite group of disease detectives known as the Epidemic Intelligence Service.
Looking for answers, CSI-style
Although agricultural toxins were proposed as a possible factor, the team ruled them out based on the prevalence of this disease only in specific coastal populations. Genetic mutations, as the sole cause, were also excluded because of the relatively recent emergence of this disease (in decades versus centuries, which is typical of inherited genetic disorders) and a sharp increase in cases in the region.
“Although it was thought to be a chronic condition, after we reviewed hundreds of clinical records and conducted surveillance for new cases, we were struck by the acute ‘flu-like’ presentation in the initial stages of this disease. At the onset, the disease looked remarkably like a classic hyper-inflammatory response to an infection. We screened for several infectious agents, but could not pin it down to any one in particular,” said Murray, who also is the assistant dean at the National School of Tropical Medicine at Baylor and Vice Chair for Research in the Department of Pediatrics at Texas Children’s.
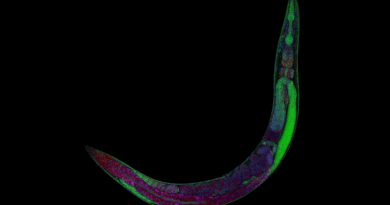
The team then turned its attention to clinical and pathological tests that led them to the most important clues to crack this case. Most affected individuals had recently developed anemia and their kidney biopsies showed extreme inflammation in the tubules and cortico-medullary junctions of the kidney, indicative of heavy metal or trace element toxicity. The pieces of the puzzle were finally coming together.
Dr. Rebecca Fischer, who was Dr. Murray’s postdoctoral fellow at the time and now assistant professor of epidemiology at Texas A&M University, worked to pull together these complex analyses, and nephrologists, Drs. Sreedhar Mandayam and Chandan Vangala at Baylor, helped to guide the team in their clinical interpretation of acute cases.
The team then collaborated with Drs. Jason Unrine and Wayne Sanderson at the University of Kentucky who specialize in trace element toxicity. The easiest way to test the levels of heavy metals is by analyzing toenails. The researchers collected toenail clippings of individuals about three months after they experienced an acute kidney injury event and analyzed the clippings for 15 trace elements, including heavy metals. Most importantly, they compared these analyses to controls they recruited from the same population who had no evidence of kidney disease.
Finding answers
They found affected cases to have significantly increased levels of nickel. They also identified higher levels of aluminum and vanadium in affected cases than control subjects, but nickel was by far the strongest correlate, and biologically, it made sense with the clinical presentation.
Nickel is an abundant, naturally occurring heavy metal and like iron, it is essential for the human body, but is needed only in trace quantities. Excess recurrent exposure to nickel, by incidental ingestion through contaminated water, food or soil, can cause several toxic and carcinogenic effects.
People who work a lot with soil, such as agricultural field laborers, miners and brick-makers, had the highest risk of acquiring this disease, leading the researchers to theorize that the source of nickel exposure was likely geologic in nature. It is also possible, the researchers propose, that the exposure is linked to a volcanic chain in the area that became active in the late 90s, after which incidences of this chronic kidney disease began to skyrocket in lowland areas downstream from the volcanoes in this chain.
“While we still need to validate these findings in other areas impacted by MeN, such as El Salvador or Guatemala, and to confirm the geologic source of nickel contamination, we are very excited to have found a strong lead in this challenging public health problem,” Murray said.
This work provides new, compelling evidence that low-dose exposure to nickel can cause systemic inflammation, anemia and kidney injury – hallmarks of acute MeN that progresses to chronic kidney disease in around 90 percent of the patients.
This study led to the implementation of several public health strategies, such as finding ways to protect drinking water sources from soil and runoff water contamination and educating community members about the need to wash their hands frequently after working with soil.
It is gratifying to see our efforts are starting to pay off. After the implementation of these measures, we noticed a dramatic reduction in the number of new cases, an indication that we are moving in the right direction,” Murray said.
“This is the first-ever downward trend in this outbreak since its emergence two decades ago. Considering the sobering death toll in the affected communities, I am relieved we can finally do something about it.”
Find all the details of this work in the journal PLoS ONE.
The authors were affiliated with one or more of the following institutions: Baylor College of Medicine, Texas Children’s Hospital, Texas A & M, University of Kentucky and M.D. Anderson Cancer Center.
The study was partially funded by the El Comité Nacional de Productores de Azúcar de Nicaragua (CNPA) and the National Institutes of Health.
Read more here.