New insights into the mediators of patient recovery after CAR T cell immunotherapy
A child with rhabdomyosarcoma, a form of muscle cancer, that had spread to the bone marrow, showed no detectable cancer after treatment with a novel form of immunotherapy consisting of chimeric antigen receptor (CAR) T cells that were engineered to target the HER2 protein on the surface of the cancer cells.
The clinical trial, conducted by researchers at Baylor College of Medicine, Texas Children’s Hospital and Houston Methodist Hospital, also provides new insights into how this exceptional recovery occurred.
“This child’s cancer was considered high risk because it had not responded to standard chemotherapy. As a result, this child was a candidate to receive a promising new CAR T cell therapy, a personalized form of immunotherapy that redirects the patient’s own immune T cells to recognize and fight the tumor,” said first and corresponding author Dr. Meenakshi Hegde, assistant professor of pediatric hematology-oncology at Baylor College of Medicine and Texas Children’s.

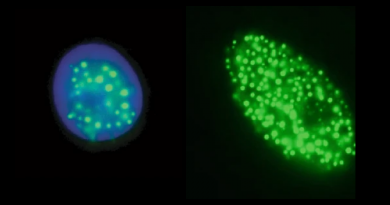
About 75 percent of the tumor cells in this patient displayed a protein on their surface called HER2. The researchers reprogrammed the T cells to target the HER2 protein by genetically engineering them to express CAR molecules that recognize the HER2-expressing (HER2+) cancer cells.
In a previous clinical trial, the HEROS study, the researchers found that CAR T cells directed at HER2+ tumor cells had a favorable safety profile. This early generation CAR T cell treatment resulted in clinical benefit in a small subset of patients, but it did not eradicate their tumors.
“From the HEROS trial, we learned that HER2-CAR T cells expanded but did not persist in the patients, which could in part explain the lack of anti-tumor responses,” said Hegde, who also is part of Baylor’s Dan L Duncan Comprehensive Cancer Center.
To overcome this limitation, in the HEROS 2.0 trial Hedged and her colleagues added successive HER2-CAR T cell infusions along with low-dose chemotherapy to eliminate normal T cells as a strategy to improve the expansion and persistence of the infused HER2-CAR T. The T cell-depleting chemotherapy administered before transferring HER2-CAR T cells eliminated the patient’s existing immune cells, creating a space for the engineered CAR T cells to expand in the patient.
“Although the child had a lasting response to HER2-CAR T cells with no tumor detected, the cancer returned six months after we stopped the T cell infusions. Fortunately, the child achieved a second remission after retreatment with HER2-CAR T cells,” Hegde said. “Considering the several challenges in successfully treating solid tumors using CAR T cells, achieving this exceptional tumor response is very encouraging.”
At the time of this report, the child is 19 months off T cell treatment and remains healthy and cancer free.
New insights into how this exceptional recovery occurred
The sustained tumor response in this child has provided the researchers important insights into how the cancer was eliminated. The CAR T cells were engineered to recognize and attack HER2+ cancer cells. Although not all cancer cells expressed HER2 on the cell surface, the tumor was eliminated in its entirety prompting the question of how the HER2-negative cancer cells were eradicated.
We found evidence suggesting that, following the infusion of HER2-specific CAR T cells, the patient’s own immune system was recruited to act against the tumor, which might help explain the durable complete response,” Hegde said.
“We plan on conducting more detailed experiments in a larger group of patients treated with HER2 CAR T cells to better understand the involvement of the patient’s immune system in eliminating the cancer.”

“It is fascinating to see remodeling of the patient’s T cell compartment and development of antibodies directed against proteins implicated in tumor survival and metastasis during the course of treatment in this child. The immune activation mechanisms and associated tumor targets that unfolded during the acquired response could inform novel approaches to fight difficult-to-treat cancers,” said Dr. Sujith Joseph, senior scientist at Baylor’s Center for Cell and Gene Therapy, who conducted the in depth evaluation of the patient’s immune response.

“This study shows that CAR T cells could perhaps act as vaccines by exposing cancer proteins to the patient’s immune system. With more understanding and further refinement of their design, CAR T cells could be effective against some incurable malignancies,” said senior author Dr. Nabil Ahmed, associate professor of pediatrics and immunology at Baylor and Texas Children’s Hospital.
Read the complete study in the journal Nature Communications.
Other authors who also contributed to this work include Farzana Pashankar, Christopher DeRenzo, Khaled Sanber, Shoba Navai, Tiara T. Byrd, John Hicks, Mina Xu, Claudia Gerken, Mamta Kalra, Catherine Robertson, Huimin Zhang, Ankita Shree, Birju Mehta, Olga Dakhova, Vita S. Salsman, Bambi Grilley, Adrian Gee, Gianpietro Dotti, Helen E. Heslop, Malcolm K. Brenner, Winfried S. Wels and Stephen Gottschalk. The authors are affiliated with one or more of the following institutions: Baylor College of Medicine, Texas Children’s Hospital, Houston Methodist Hospital, Yale University School of Medicine, Frankfurt’s Institute for Tumor Biology and Experimental Therapy, German Cancer Consortium and Goethe University, St. Jude’s Children’s Hospital.
The trial was supported by Stand Up To Cancer© (SU2C) – St. Baldrick’s Pediatric Cancer Dream Team Translational Research Grant (SU2C-AACR-DT1113), Alex’s Lemonade Stand Pediatric Cancer Foundation, Cancer Prevention Research Institute of Texas (CPRIT) grant (RP101335), The V Foundation for Cancer Research, Triumph Over Kid Cancer (TOKC), and by Cookies for Kids’ CancerTM Foundation. Further support was provided by the Clinical Research Center at Texas Children’s Hospital, shared resources through Dan L. Duncan Cancer Center Support Grant P30CA125123, the National Cancer Institute of the National Institute for Health (NIH) under the Cancer Moonshot U54 project 1U54CA232568-01, the State of Texas CPRIT training program RP160283 at Baylor College of Medicine and the National Cancer Institute of the NIH award number K12CA090433.