These 300,000 cells can improve our understanding of chronic lung disease
Despite substantial progress in the understandig of pulmonary fibrosis (PF) in laboratory animals, researchers have a limited perspective of the cellular and molecular processes that determine the characteristics of lungs with the condition.
Dr. Ivan Rosas at Baylor College of Medicine, Dr. Naftali Kaminski from Yale School of Medicine and colleagues have taken a major step toward a deeper appreciation of pulmonary fibrosis and other chronic pulmonary diseases such as chronic obstructive pulmonary disease (COPD).

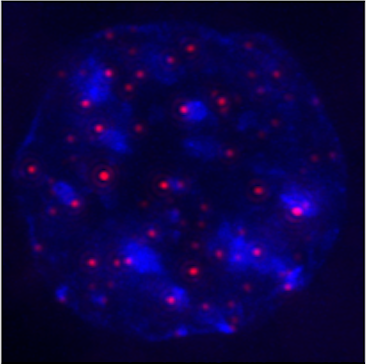
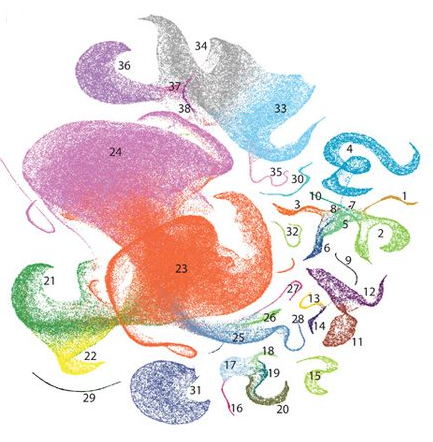
They developed the largest single-cell data set of a chronic lung disease by sequencing the RNA of more than 300,000 cells from lungs affected with these conditions. The results, published in the journal Science Advances, offer an online cell atlas that allows the public to explore the individual cells in lungs with the diseases.
“This is a technological accomplishment and is a new perspective on the two diseases, but it is also the starting point for analysis that will lead to a better understanding of the disease and the development of therapy,” said Rosas, the co-lead researcher and co-senior author of the study and chief of pulmonary, critical care and sleep medicine in the Department of Medicine at Baylor.
Rosas explains that the cell atlas was achieved by separating all the cells within the lung and then measuring RNA expression in each individual cell. Although this method has been done for other diseases, this is the largest single-cell gene expression dataset that has been completed in a chronic lung disease.
“When we analyzed the data we were surprised by how dramatically different were cells obtained from patients with PF from all other lungs – we actually found cells that were not described before, and this may have significant implications on diagnosis and management for the disease,” said Kaminski, the co-senior author on the study and chief of pulmonary, critical care and sleep medicine at Yale.
“This data is now publicly available so it’s going to broadly impact science and these diseases,” Rosas said. “People can now download the data set and conduct their own independent analysis and research.”
Because physicians need a further understanding of chronic lung diseases like PF, Rosas explains that having a large and accessible data set of PF or COPD cells is an essential tool to begin developing therapies to target the disease.
Rosas led the study during his time at Harvard Medical School in Boston. The studies on PF will continue in laboratories at Baylor College of Medicine.
“Chronic lung diseases are one of the leading causes of morbidity and death in diagnosed patients, but this innovative technology is the starting point for more pointed research in terms of the pathogenesis and the mechanisms of the disease and also the potential therapy that could be derived from the information,” Rosas said.
The research is funded by the NIH National Heart, Lung, and Blood Institute and a $1 million gift from the venture philanthropy group Three Lakes Partners, whose mission is to accelerate progress in IPF research.