Premature epigenomic aging acts like a ‘sleeper cell’ that is awaken by Western-style diet
The epigenome is sometimes referred to as the “software” or “operating system” of the genome. It comprises small chemical modifications to DNA and the proteins that make up our chromosomes, and controls the activity of all the genes within the genome.

During early life, as our organs develop, the epigenome guides and changes along with normal developmental milestones. Exposure to endocrine-disrupting chemicals (EDCs) during this process can cause widespread reprogramming of this “software,” and this reprogramming persists for the life of the individual. Depending on the organ, the window of vulnerability for this reprogramming may be anytime from development in the womb to childhood and adolescence, depending on how long normal development lasts.
“In this study, we found that even brief exposure to certain chemicals while the liver is developing, prematurely aged the liver epigenome. Exposure to these EDCs caused the young liver to acquire an adult epigenomic signature,” said Dr. Cheryl Walker, professor and director of the Center for Precision Environmental Health at Baylor and lead author on the study. “However, this premature aging of the epigenome did not have an effect on health until later in life and after exposure to a high-fat diet.”
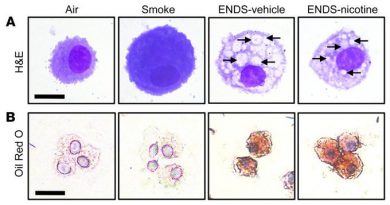
In a healthy liver, the epigenome goes through a normal aging process. In this study, after exposure to an EDC, the researchers saw that this process accelerated. So, a 6-day old rat had the same epigenome they would normally see in an adult rat.

“The effect of this change on metabolic function wasn’t immediate; instead, it was like a ticking time bomb, which was only ignited when we switched the animals to a Western-style diet, high in fat, sugar and cholesterol,” said Walker, who also is the Alkek Presidential Chair in Environmental Health at Baylor.
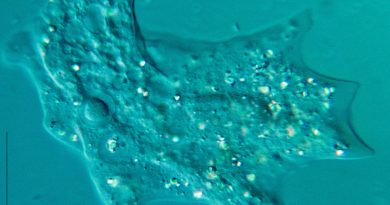
Rats that were exposed early to EDC and later to a Western-style diet were found to be more susceptible to metabolic dysfunction than those that had the same EDC exposure, but were kept on a healthy diet. Those that remained on a healthy diet, despite the fact their epigenome had been reprogrammed, did not show the same changes in expression of genes that control metabolism, or accumulation of lipids in their serum, seen in rats on the high fat, sugar and cholesterol diet.
This study shows us how environmental exposures affect our health and disease susceptibility, both early and later in life,” Walker said. “It also shows us that some people may be more adversely affected by a high-fat diet as adults than others due to environmental exposures they experienced earlier in their life.”
Read all the details of this work in Nature Communications.
Featured as the June paper of the month by the National Institute of Environmental Health Sciences (NIEHS), this work was supported as part of the NIEHS multi-phased Toxicant Exposures and Responses by Genomic and Epigenomic Regulators of Transcription (TaRGET) Program. While these findings are only in lab models at this time, researchers hope this and similar studies being conducted by the TARGET II Consortium can lead the way to identifying biomarkers to help better predict who is at risk for metabolic dysfunction such as fatty liver disease, diabetes or heart disease, and allow for more precise and early interventions.
Others who contributed to the work include Lindsey S.Treviño, Jianrong Dong, Ahkilesh Kaushal, Tiffany A.Katz, Rahul Kumar Jangid, Matthew J.Robertson, Sandra L.Grimm, Chandra Shekar R. Ambati, Vasanta Putluri, Aaron R.Cox, Kang Ho Kim, Thaddeus D.May, Morgan R.Gallo, David D. Moore, Sean M. Hartig, Charles E.Foulds, Nagireddy Putluri, Cristian Coarfa. For affiliation please see the full publication in Nature Communications.
This work was supported in part by NIH grants U01ES026719, 1P30ES030285, R01ES023206 and R01DK114356; American Diabetes Association grant #1-18-IBS-105 and a sub-award from NIH grant U24DK097748. Lipidomics and metabolomics sample processing and analysis were conducted by the Metabolomics Core at Baylor College of Medicine supported by CPRIT Proteomics and Metabolomics Core Facility funding (RP170005), the NIH (P30 CA125123) and the Dan L Duncan Cancer Center at Baylor College of Medicine.