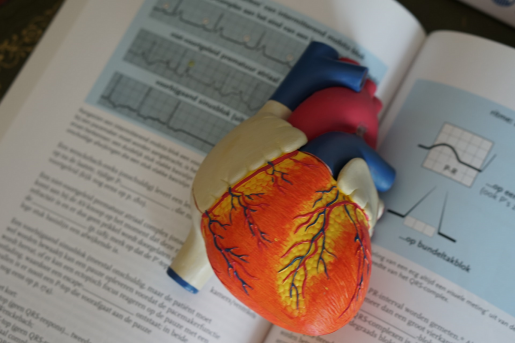
COVID-19 and advanced heart and lung disease
As a heart and lung transplant surgeon who routinely treats end-stage disease, I have been studying the effect of COVID-19 on the heart and lungs, and I wanted to provide some perspective on what we know so far.
This virus enters our body through mucous membranes and epithelial cells of the eyes, nose and throat, typically. It then works its way down to the lungs. In the lungs, it enters the main cells that line the lung such as epithelial and endothelial cells that allow gas exchange and interstitial cells that give the lung elasticity.
The body mounts a major inflammatory response that leads to muscle aches, fevers, and sometimes heart cell dysfunction. This reduces the ability of the heart to pump well. At times, it can affect other organs.
So what does this mean in our modern era of advanced heart and lung support medicines and mechanical assistance devices?
Here’s one way to look at it.
The virus sets up shop in the lung cells and re-programs the cells to reproduce the virus and ultimately kill the cell. The good news is the lung has an incredible ability to repopulate itself with healthy new cells.
How do we turn it around? Time is the number one tool we need when we face a serious lung infection with COVID-19.
What do we do in the meantime? It all depends on the amount of lung affected and the person’s reserve. Let’s say broadly speaking a third of the lung is affected. If you have plenty of healthy lung you will be fine. You’ll feel a little short of breath and you may need a little oxygen through the nose.
Having a pulse oximeter at home can be a useful way to determine if you need to come into the hospital. A saturation reading of less than 90% suggests you will need some additional oxygen. With time and minimal support your lung will recover.
What if it affects between 33% and 66% of the lung?
This is more dangerous. Whether or not you have reserve, you may need a lot more oxygen therapy. This means you may need a ventilator. You will need more time for the lung to fight the virus and for it to regenerate healthy cells. This may take two weeks or more.
What if more than 66% of the lung is affected?
A ventilator may not be enough. You may need exteacorporeal membrane oxygenation (ECMO), which is essentially a large IV that delivers oxygen directly to your blood stream. These are in limited supply. Typically, ECMO is only done in tertiary or quaternary referral centers like the Texas Medical Center. At best, any one hospital may have 8 to 10 units available to support patients. Thankfully, this is not needed that often.
How long can you stay on ECMO?
As long as needed. The virus will lead to some systemic effects outside of the lung. The extent to which other organs are affected determines the effectiveness of ECMO. If it remains primarily a lung issue, then ECMO will give all the time and support needed for the lung to heal. If the blood pressure starts to lose its vascular tone, the kidneys start to fail, or the liver starts to fail, then ECMO begins to lose its effectiveness.
What about the heart?
If we assume heart cells are dysfunctional but not dead, the heart may need some temporary support. This comes in three varieties, including:
- Medicine such as epinephrine that helps heart cells pump as efficiently as possible
- Medications and pacing devices that help the heart keep a normal rhythm. Medications include amiodarone, lidocaine, digoxin and devices may include a temporary pacing wire
- Devices that support the heart. The intra-aortic balloon pump is the least invasive. ECMO is another option, but the type of ECMO used for the heart is different than the lung. This type of ECMO requires a line into the venous system and the arterial system.
There are other modes of support for the heart that we use often in the setting of a heart attack or other reason for heart failure. The key is time and prevention of damage to other organs. Interestingly, it’s not so much the virus itself that affects the heart cells but rather the immune response. For this reason, anti-inflammatory medicines to dampen the immune response may be used on some occasions.
Is it safe to receive a transplant during the pandemic?
The answer depends on the hospital’s ability to contain and separate COVID-19 cases from transplant recipients. If the recipient’s path to recovery from the ICU to home is carried out in a way that takes the most precautions, then it is reasonable to consider a transplant.
Patients prior to transplant have lungs that are susceptible to a lethal viral infection. After transplant, the new lung is much healthier but immunosuppression could make it easier for the virus to infect the host. We do not yet know if this is better or worse than infection of the native lungs.
We have more options today to treat people with advanced heart and lung disease secondary to a viral infection than we ever have before. Early recognition and transfer to higher levels of care can be life-saving. Time is the biggest antidote that we currently have and the type of support needed to weather the storm depends on the degree of injury to the lungs, the heart and other organs.
-By Dr. Gabriel Loor, associate professor of surgery-cardiothoracic transplantation and circulatory support in the Michael E. DeBakey Department of Surgery at Baylor College of Medicine