Tuberous sclerosis: it’s not all about mTORC1
mTORC1, a protein complex that regulates cell metabolism, has long been considered the major driving force behind tuberous sclerosis. New experimental evidence, however, is challenging this traditional view of the disease and the implications can potentially benefit patients who partially respond to current therapies focused on mTORC1.
“Tuberous sclerosis is a rare genetic disease that causes benign tumors to grow in the brain, kidneys, skin and other organs. Patients present with a combination of symptoms that can include seizures, developmental delay, skin abnormalities and kidney disease,” said first and co-corresponding author Dr. Rituraj Pal, postdoctoral associate of molecular and human genetics at Baylor College of Medicine.

Tuberous sclerosis is caused by mutations in the genes TSC1 and TSC2. The current thought is that the dysfunctional proteins produced by these mutated genes fail to regulate mTORC1, which then becomes hyperactive and leads to the development of the disease. How the disease actually develops is still not clear.
“Previous studies have associated tuberous sclerosis with excessive accumulation of glycogen, a main source of energy, inside cells, although this has not been clearly shown,” said corresponding author Dr. Marco Sardiello, assistant professor of molecular and human genetics at Baylor and a member of the Jan and Dan Duncan Neurological Research Institute at Texas Children’s Hospital. “We know from other conditions that glycogen accumulation damages cells.”
Cells are like homes. Both are constantly producing waste that must be disposed of to keep a healthy, functional environment. Even materials that are usually not toxic, such as glycogen, will become so if they accumulate inside the cell. To gain insights into how the disease happens, the researchers first investigated whether glycogen accumulated inside cells with the disease.
Discovering a second player in tuberous sclerosis
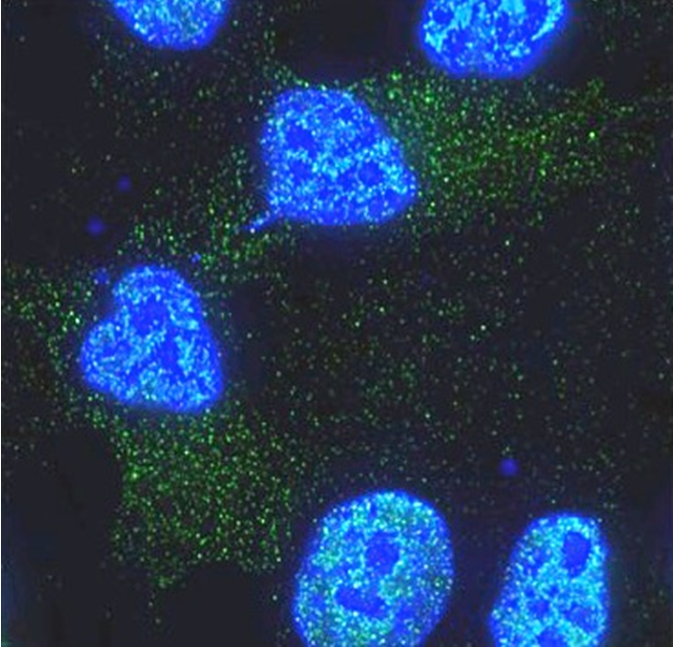
“We clearly show that glycogen accumulates inside both human and mouse cells with the condition,” Pal said. “Then we investigated the mechanism.”
The researchers looked at mTORC1, the only player that was known to be contributing to tuberous sclerosis, and found that in some cases in which the TSC2 gene is completely deleted, mTORC1 is hyperactive and partially responsible for the accumulation of glycogen.
But when the researchers tested samples from patients carrying two particular TSC2 mutations that do not completely eliminate the gene but just change the protein, they observed that mTORC1 was working normally, yet glycogen accumulated inside the cells. This suggested that there was another glycogen-clearing mechanism at play and that it was independent of mTORC1.
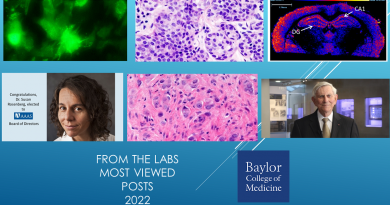
“One clue about what the second mechanism might involve was the observation that the affected cells had fewer lysosomes than normal cells,” Pal said. “Lysosomes are structures in charge of clearing cellular waste. When lysosomes fail and cellular waste accumulates, disease follows.”
Further investigations showed that the second mTORC1-independent mechanism involved defects in the formation of lysosomes and in the process that digests cellular materials, including glycogen. And this led to the accumulation of glycogen inside the cells.
Our findings put forward a new perspective on this disease that can have implications for patient treatment. We show that mutations of TSC2 are not all equal, implying that the same is true for patients,” Pal said.
Current treatments are focused on modifying only mTORC1 activity. This work suggests that further studies are needed to systematically analyze the TSC mutations carried by each patient. Some patients may be carrying TSC mutations that affect mTORC1. But in other patients TSC mutations may be affecting the second mechanism without disrupting mTORC1.
“This could lead to the development of novel approaches to treat the disease that might improve the response of patients who partially respond to the treatments focused on targeting mTORC1,” Sardiello said.
Interested in reading all the details of this work? Find them in the Proceedings of the National Academy of Sciences U.S.A.
Dr. Yan Xiong at Baylor College of Medicine also contributed to this work.
Financial support was provided by National Institutes of Health grant NS079618.