Baylor included in recent studies on best treatments for limb salvage
Two impactful trials on treating and preventing limb loss were recently published, including one study largely conducted at Baylor College of Medicine.
PROMISE II
 PROMISE II investigated a new, minimally invasive treatment approach called transcatheter arterialization of the deep veins (TAD). The purpose of the procedure is to prevent major limb amputation by creating a connection between an artery and a vein to deliver oxygenated blood to the foot in patients with chronic limb-threatening ischemia, formerly called critical limb ischemia, who have no other options for revascularization. Chronic limb-threatening ischemia is a disease where arterial blockages result in inadequate blood flow to the limbs, which may ultimately lead to amputation if not treated.
PROMISE II investigated a new, minimally invasive treatment approach called transcatheter arterialization of the deep veins (TAD). The purpose of the procedure is to prevent major limb amputation by creating a connection between an artery and a vein to deliver oxygenated blood to the foot in patients with chronic limb-threatening ischemia, formerly called critical limb ischemia, who have no other options for revascularization. Chronic limb-threatening ischemia is a disease where arterial blockages result in inadequate blood flow to the limbs, which may ultimately lead to amputation if not treated.
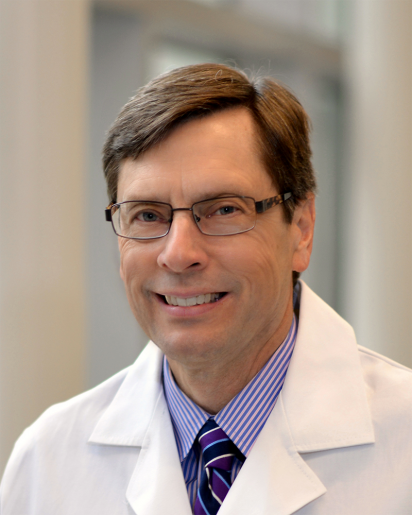
Baylor College of Medicine had the largest number of patients enrolled in the study. Dr. Joseph L. Mills Sr., professor and chief of the Division of Vascular Surgery and Endovascular Therapy, co-authored the findings in an article titled “Transcatheter Arterialization of Deep Veins in Chronic Limb-Threatening Ischemia” in the New England Journal of Medicine.
The study enrolled 105 patients with nonhealing ulcers and no available conventional surgical or endovascular revascularization treatment options.
“The study showed that TAD is a safe and successful option for patients with chronic limb-threatening ischemia who are facing the prospect of leg amputation and have no other available conventional surgical or endovascular revascularization treatment options,” Mills said.
BEST-CLI Trial
 The BEST-CLI trial, recently published in the New England Journal of Medicine, compared two different treatments for treating chronic critical limb ischemia, now called chronic limb-threatening ischemia.
The BEST-CLI trial, recently published in the New England Journal of Medicine, compared two different treatments for treating chronic critical limb ischemia, now called chronic limb-threatening ischemia.
The study compared two treatment strategies: a lower extremity bypass versus an endovascular (or minimally invasive) approach. The study found that if the surgeon determines the patient has a sufficient greater saphenous vein, then bypass is the best option for treating the disease. If a patient does not have a saphenous vein that would be viable for the procedure, then minimally invasive techniques have similar outcomes to the bypass.
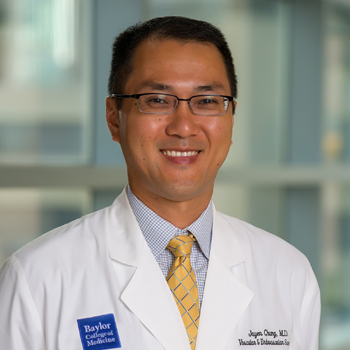
“The greater saphenous vein is a large vein that runs from the foot all the way up to the groin,” says Dr. Jayer Chung, associate professor of surgery in the Division of Vascular Surgery and Endovascular Therapy. “During a bypass procedure, the surgeon takes a segment of this vein and attaches it to the artery above and below the blockage, allowing blood to flow around the blocked area. This trial was very impactful because we now know that patients with critical limb ischemia who lack sufficient vein for the bypass can have the option of endovascular therapy with comparable outcomes.”
STEP program
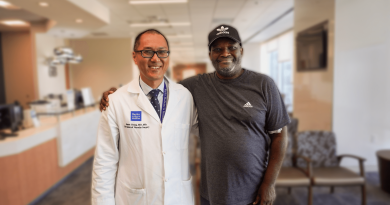
Vascular surgeons at Baylor Medicine can perform traditional bypass surgery as well as innovative, advanced endovascular techniques. They work in tandem with podiatrists in the Save the Extremity Program (STEP) so the patient has comprehensive care to maximize the preservation and function of the limb.
In fact, Jay Netherly, a Houston resident and diabetes patient, avoided foot and leg amputation with the help of the specialists in STEP. Read his full story here.
By Tiffany Harston, communications associate with the Michael E. DeBakey Department of Surgery