Brain stimulation device enables new understanding of OCD
A team of researchers surgically implanted brain stimulators in five patients with severe obsessive-compulsive disorder (OCD) to not only treat their disabling symptoms but also – for the first time – to simultaneously record and wirelessly stream brain signals.
Katie’s story
Katie, one of the patients, suffered from debilitating OCD for years. After enduring a health crisis in 2014, her symptoms became unbearable. Her fear of contamination immensely grew to the point where she would not allow anyone in her home and she would obsessively deep clean her house. She recalls a time where she spent 17 hours in her bathroom, cleaning it endlessly, compulsion after compulsion, unable to stop.
“OCD is so frustrating because you understand rationally that this doesn’t make sense, but the fear that something bad could happen to someone I loved outweighed the rational side of it,” Katie said. “Once it was all-encompassing, I tried different therapies: a partial hospitalization program, hours of intensive exposure response prevention therapy and different medications. Through all of that, the OCD just grew until I was completely debilitated by it.”
To qualify for deep brain stimulation (DBS), you must have severe, chronic, treatment-resistant OCD. As different treatments failed her, Katie was determined to rid herself of the hopelessness. Her urgency to regain a normal life led her to participate in this study.
Deep brain stimulation
“We carefully look at the records to make sure the patients have had adequate medication trials, as well as OCD-specific behavioral therapy to qualify as treatment-resistant,” said Dr. Wayne Goodman, D.C. and Irene Ellwood Chair in Psychiatry and professor in the Menninger Department of Psychiatry and Behavioral Sciences at Baylor College of Medicine. “We want to make sure that a wide range of appropriate non-surgical therapies have been tried before proceeding with DBS.”


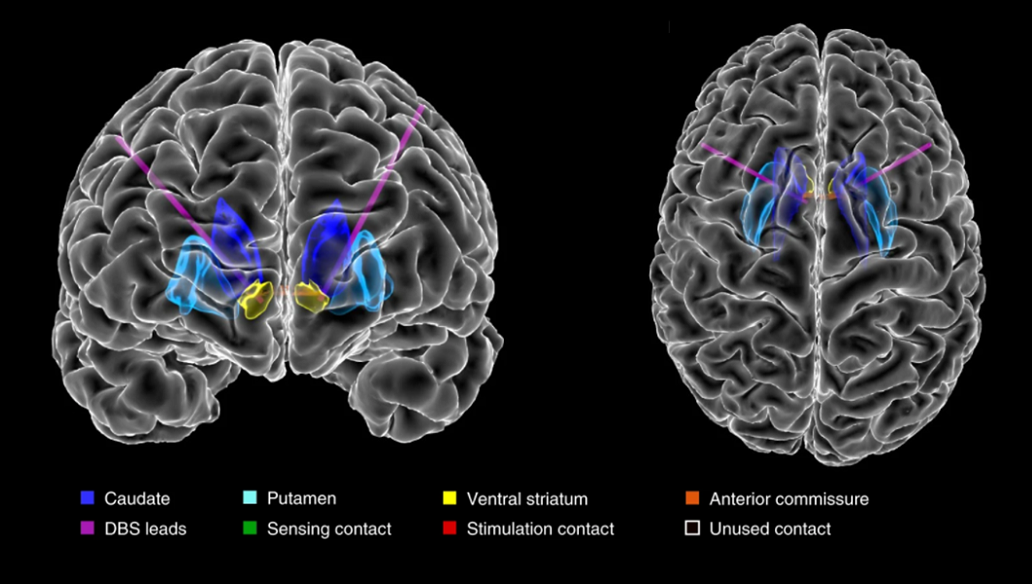
The DBS device was surgically implanted in five study participants by Dr. Sameer Sheth, associate professor of neurosurgery, Cullen Foundation Endowed Chair, McNair Scholar, and vice chair of research in the Department of Neurosurgery at Baylor. During electrode placement in the brain, patients were awake part of the time while answering questions about how they felt when the stimulation was turned on. This information allowed the research team to fine-tune the positioning of the electrodes in the brain. After surgery, patients visited Goodman at least once a month for optimization of DBS therapy during simultaneous brain recordings. In between visits, patients used a tablet application developed by Brown University researchers to collect brain recordings during daily activities at home.
What is unique about this device is that it not only stimulates, but it can record brain activity,” said Sheth.
“Our goal is to understand what those brain recordings are telling us and to train the device to recognize certain patterns associated with specific symptoms. The better we understand the neural signatures of health and disease, the greater our chances of using DBS to successfully treat challenging brain disorders like OCD.”
“We were able to analyze over 1,000 hours of brain recordings, synchronized with symptom ratings. The Brown team was responsible for analyzing that data to try to establish a relationship between the recorded brain signals and how the patient is feeling,” said Dr. Nicole Provenza, lead author, recent Brown biomedical engineering doctoral graduate and current postdoctoral fellow in the Department of Neurosurgery at Baylor.
Noticeable improvement
Katie, who had the surgery over a year ago, felt immediate changes in the way her brain processed OCD after stimulation was turned on.
Since her surgery, Katie spends more time with her loved ones again and feels hope for a future that is not ruled by OCD.
“Before the surgery, I felt truly hopeless. I felt that I was at the end and didn’t know how I could keep trying to survive this. The amount of pressure felt so massive, I just felt like I was crumbling underneath it and there was no way out. The surgery and device have changed my life. I have hope again and am starting to do the things I love,” Katie said.

“Thanks to Katie and the other patients’ efforts completing daily recordings at home, we were able to identify candidate trends between brain activity and OCD symptom severity,” said Dr. David Borton, associate professor of biomedical engineering at Brown University. “In the future, these biomarkers could be used to enable adaptive DBS systems that are able to automatically adjust stimulation levels in response to fluctuations in symptoms.”
“In addition to advancing DBS therapy for cases of severe and treatment resistant OCD, this study has the potential for improving our understanding of the underlying neurocircuitry of the disorder,” Provenza said.
This deepened understanding may allow us to identify new anatomic targets for treatment that may be amenable to novel interventions that are less invasive than DBS,” Provenza said.
Find all the details of this work in the journal Nature Medicine.
This research was in collaboration with Brown University, the University of Pittsburgh and Carnegie Mellon University. Other authors include Eric Storch, Evan Dastin-van Rijn, Raissa Mathura, Yaohan Ding, Gregory Vogt, Michelle Avendano-Ortega, Nithya Ramakrishnan, Noam Peled, Luiz Fernando Fracassi Gelin, David Xing, Laszlo Jeni, Itir Onal Ertugrul, Adriel Barrios-Anderson, Evan Matteson, Andrew Wiese, Junqian Xu, Ashwin Viswanathan, Matthew Harrison, Kelly Bijanki and Jeffrey Cohn.
The research was supported by the National Institute of Neurological Disorders and Stroke’s BRAIN Initiative (UH3NS100549 and UH3NS103549), the Charles Stark Draper Laboratory Fellowship, the McNair Foundation, the Texas Higher Education Coordinating Board, the National Institutes of Health (1RF1MH121371, U54-HD083092, NIH MH096951, K01-MH-116364 and R21-NS-104953, 3R25MH101076-05S2, 1S10OD025181) and the Karen T. Romer Undergraduate Teaching and Research Award at Brown University.
*Editor’s note: The study participant prefers to use her first name, Katie, for interviews.
Learn more about psychiatry and behavioral health outpatient services at Baylor Medicine, or call 713-798-4857 to schedule an appointment.
By Homa Shalchi