Making strides in tackling osteoarthritis
Osteoarthritis (OA) is a progressive disease of the flexible joints. It is the most common joint disorder in the U.S., ranking among the top three causes of chronic disability and delay in returning to work. OA accounts for more difficulty with climbing stairs and walking than any other disease. It also is the most common reason for total hip and total knee replacement.

“OA develops when the smooth cushion between bones, the cartilage, breaks down. Progressively, joints become painful, swollen and hard to move,” said Dr. Prathap Jayaram, director of regenerative sports medicine in the Department of Physical Medicine and Rehabilitation at Baylor College of Medicine and first author of a current study focused on the disease-modifying effects of a treatment called platelet-rich plasma (PRP).

Currently, OA patients only have options for treatments limited to relieve pain with nonsteroidal anti-inflammatories and intra-articular steroid injections. However, research on therapies with the potential to alter OA progression and promote joint repair is underway. Platelet-rich plasma is one of the promising candidates to treat OA that are currently being used in clinical practice.
“PRP is prepared from the patient’s own blood by removing the red blood cells and enriching the concentration of platelets,” Jayaram said. “PRP also contains white blood cells, or leukocytes. PRPs are formulated either leucocyte-rich or leukocyte-poor, but their effects on OA have not been comprehensively assessed directly.”
In this study, Jayaram and members of the lab of Dr. Brendan Lee, Robert and Janice McNair Endowed Chair and professor of molecular and human genetics at Baylor, were the first group to demonstrate potential disease-modifying effects of PRP that correlate with functional outcomes.
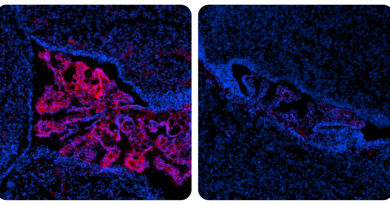
The group is among the first to assess in preclinical models clinically relevant formulations of platelet-rich plasma that can delay osteoarthritis progression and improve pain. They compared the effect of leucocyte-rich-PRP and leucocyte-poor-PRP in animal models of OA, assessing the effect of the different PRP formulations on chronic pain and on disease development, according to microscopic evaluation of the joint tissue.
The results
The researchers found that while leukocyte-poor-PRP and to a lesser extent leukocyte-rich-PRP protected from cartilage loss, significant tissue damage remained within OA joints. The results also suggested that PRP therapy seemed to affect OA progression and pain associated with the condition and that the effects may be leukocyte-dependent.
“The results of our study support the safety profile of PRP and highlight some potential beneficial effects of PRP therapy for treatment of OA. At the same time, differences we observed between leukocyte-poor-PRP and leucocyte-rich-PRP in terms of their protective and analgesic properties point toward compositional and mechanistic complexities that remain unknown,” Jayaram said. “Future work is needed to understand how the different components of PRP affect OA development and pain and how these could be modified to achieve greater therapeutic efficacy.”
The group is now translating these findings into clinical use at Baylor for patient care. Patients who are interested in seeking this treatment can schedule an appointment with Jayaram at 713-798-7246.
Find all the details of this study in the journal Osteoarthritis and Cartilage.
Liu, B. Dawson, S. Ketkar, S.J. Patel and M.W. Grol, all at Baylor College of Medicine, also contributed to this study.
The study was supported by the BCM Intellectual and Developmental Disabilities Research Center (HD024064) from the Eunice Kennedy Shriver National Institute of Child Health and Human Development, the Rolanette and Berdon Lawrence Bone Disease Program of Texas, the BCM Center for Skeletal Medicine and Biology, and the Pamela and David Ott Center for Heritable Disorders of Connective Tissue. Further support was provided by a PMR Foundation, ERF Matterson Grant, and by a U01 grant from the NIH.