Miniature noses to help prevent infections and promote nasal health
Our noses are home to a variety of bacteria. Some, like Staphylococcus aureus or Streptococcus pneumoniae, can cause serious infections, especially when bacteria become resistant to antibiotics. Other bacteria, like the lesser-known Dolosigranulum pigrum, often are found in healthy noses and may help keep bad bacteria at bay.
To better understand how different bacteria interact with the lining of the human nose, researchers at Baylor College of Medicine used a miniature model of the human nose to study how bacteria can live in nasal passages.

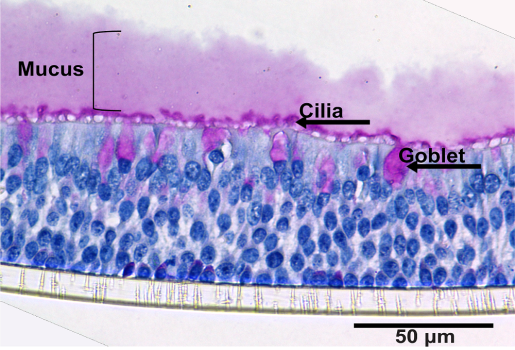
“We worked with human nasal organoids (HNOs), a laboratory-grown cell layer like the one that coats the inside of our noses, which is the point of first contact between nasal bacteria and us,” said corresponding author Dr. Katherine P. Lemon, associate professor of pediatric infectious diseases and of molecular virology and microbiology at Baylor. “In people, the cells lining the inside of the nose, the epithelium, are exposed to air on one side and to the blood circulatory system on their opposite side. Our HNO cultures produced by Baylor’s 3D Organoid Core mimic this situation.”
Researchers in the core harvest epithelium by swabbing a human nose and growing cells in the lab. Some of these cells will survive indefinitely, so they can be stored and become a long-term resource. The core then grows some of these on tissue-culture plates that provide an air-liquid interface, where the top side of the epithelium is exposed to air and the bottom side is bathed in liquid that provides nutrients to the cells.
Compared to other lab models, such as cancer-derived cell lines or animal models, HNOs offer several advantages. They very closely resemble real human nasal tissue, can be used for multiple experiments over years, and reflect the genetic diversity of human donors.


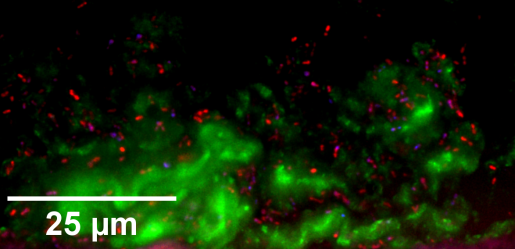
Using this model, first authors Andrea I. Boyd and Leah A. Kafer, graduate students in the Lemon lab, and their colleagues studied how different types of bacteria – S. aureus, S. pneumoniae and D. pigrum – independently colonize nasal epithelial cells and how these cells respond to bacteria.
The researchers report in mSphere, a journal of the American Society for Microbiology, that all three bacteria were able to colonize the HNOs without causing significant damage. They stayed in the mucus layer and did not invade the cells. This is important because colonization – living on the surface – is different from infection – the invading and damaging of tissue. HNOs tolerated the bacteria well, showing only minimal signs of cell stress.
“The three bacteria colonized and triggered different immune responses on the nasal cells,” Lemon said.
For instance, S. aureus caused a strong reaction, triggering nasal epithelial cells to produce interleukin-1, a type of cytokine or molecule that signals the body to respond to threats like harmful microbes with an immune response. S. pneumoniae increased levels of another cytokine, CXCL11, which also is involved in immune responses. This suggests that even without causing damage, colonizing bacteria can still stimulate the immune system.
On the other hand, D. pigrum, the beneficial bacterium, reduced the production of a cytokine called CXCL10. This molecule is involved in inflammation and immune responses. Lower levels of CXCL10 might help reduce harmful inflammation, suggesting that D. pigrum could have protective effects. All three bacteria, whether alive or dead, increased production of certain cytokines like G-CSF and CCL20. These molecules help recruit immune cells like neutrophils and lymphocytes to the site of colonization.
When people ask me, ‘What do you work on?’ I usually reply, ‘I study how good bacteria might keep bad bacteria out of people’s noses.’ The HNO model offers a new way to study these bacterial interactions in detail in children and adults. It could be used to test how different bacterial strains behave, how multiple species interact, and how the nasal microbial community, the microbiota, affects diseases like chronic sinusitis or respiratory infections.”
Other contributors to this work include Isabel F. Escapa, Amal Kambal, Hira Tariq, Susan G. Hilsenbeck, Hoa Nguyen-Phuc, Anubama Rajan, Joshua M. Lensmire, Kathryn A. Patras, Pedro A. Piedra and Sarah E. Blutt. The authors are affiliated with Baylor College of Medicine and/or Texas Children’s Hospital.
This research was supported by funding from the National Institute of Allergy and Infectious Diseases of the National Institutes for Health (NIH) under awards U19AI157981, U19AI144297, U19AI116497 and F31AI172324. Further support was provided by NIH grants (P30DK056338, DK56338, CA125123, ES030285) and institutional funds from BCM and CPRIT grants (RP150578, RP170719).