An unprecedented look at endometrial cancer
Which therapy will benefit this particular patient the most? Dr. Bing Zhang and his colleagues offer insights that might help physicians better answer this question for endometrial cancer, commonly known as uterine cancer.
Zhang, professor in the Lester and Sue Smith Breast Center and the Department of Molecular and Human Genetics at Baylor College of Medicine, teamed up with colleagues at NYU Grossman School of Medicine, the Department of Energy’s Pacific Northwest National Laboratory and Washington University in St. Louis. Together, they looked for the first time at the dozens of molecular steps that occur to bring about endometrial cancer.
“This work contributes to the personalized medicine we need to deliver for patients who have endometrial cancer,” said Zhang, a member of the Dan L Duncan Comprehensive Cancer Center, a Cancer Prevention & Research Institute of Texas (CPRIT) Scholar and a McNair Scholar at Baylor. “Such work will help us to know which patients will need aggressive treatment and offers clues about why a common treatment is not effective with some patients.”
The study, funded by the National Cancer Institute, also suggests a potential role for already-approved drugs that target proteins called CDK12, SMARCA4 and PML in other types of cancer. Zhang, is one of five corresponding authors.
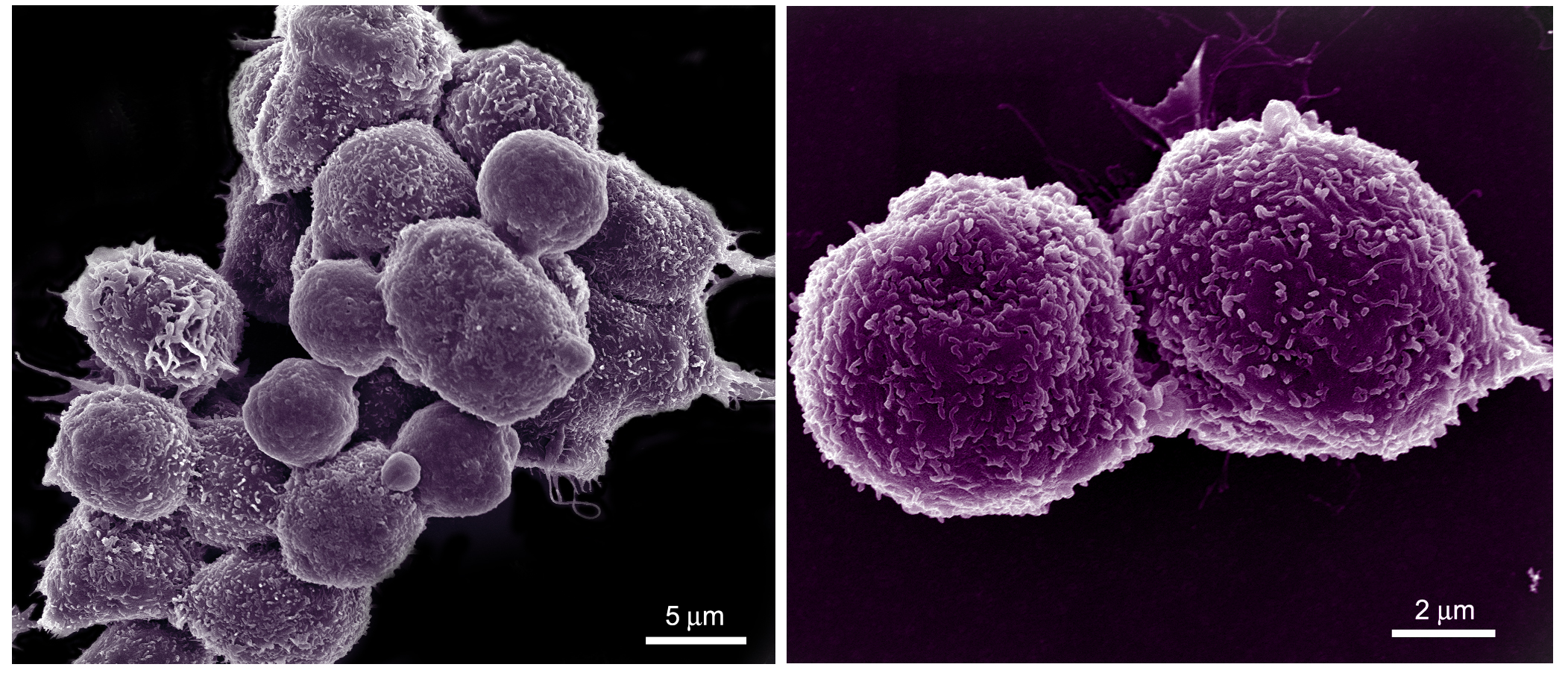
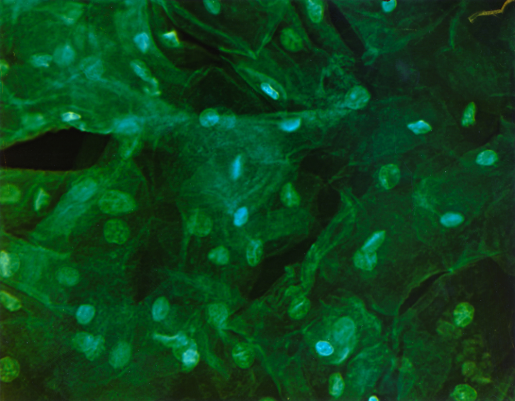
The team studied 95 uterine tumors as well as 49 normal uterine tissue samples. Scientists measured the abundance and modifications of molecular players, including DNA, messenger RNAs, circular RNAs, micro RNAs, proteins and evidence of what scientists call “post-translational modifications.” These modifications refer to the addition of specific chemical tags to proteins, including acetyl groups or phosphoryl groups, that are are key to determining when and where proteins, the molecular workhorses of every cell, are on or off. Altogether the team took more than 12 million measurements.
Identifying the most aggressive tumors
Scientists developed a promising new way to identify tumors that currently are classified as not aggressive but which turn out to be just as invasive as a serous tumor, a type of ovarian tumor which grows quickly and is more likely than other tumors to kill patients.
Right now the aggressiveness of an endometrial tumor is determined largely by viewing the cells under a microscope. The team explored an additional method, showing how the activity levels of certain proteins clearly differentiate aggressive from less-aggressive tumors. As one example, the team showed how the protein beta-catenin, a well-known actor in many types of cancer, interacts with a signaling pathway known as Wnt to evade detection, accumulate and spur cells to grow out of control.
Unexpectedly, the team also found that a process that involves packing and unpacking genes happens more often than expected in tumor cells.
With more than 7 feet of DNA squeezed into nearly every cell, the body packs it super efficiently, but it needs to unspool the DNA so that other molecular machinery can access it. The team’s measures indicate that a key part of the process, known as histone acetylation, is very active in endometrial cancer.
How cells become invasive
The team discovered that often-overlooked non-coding molecules known as circular RNAs seem to be involved in “endothelial-mesenchymal transition,” or EMT, a transformation that cells undergo when they gain the ability to spread or metastasize, which makes endometrial cancer deadly.
“This is the first report that circular RNAs may promote EMT in endometrial cancer,” said Dr. Yongchao Dou, first author of the paper and lead bioinformatics programmer in the Bing Zhang Lab at Baylor. “Interestingly, dozens of circular RNAs work together to achieve this goal.”
Identifying patients who will or won’t benefit from ‘immune checkpoint therapy’
The team created a new way to determine which patients are most likely to benefit from a treatment known as immune checkpoint therapy, where drugs like pembrolizumab and nivolumab are used to dodge the barriers that some cancer cells use to evade the immune system. It’s one of many ways that physicians are exploring the use of immunotherapy to spur the body’s natural defenses to fight cancer.
Currently in endometrial cancer, physicians use a measurement known as “Mismatch Repair Deficient” (dMMR) to determine which patients are most likely to benefit. Based on the measurements of immune activity in this study, the scientists have proposed a new measure focused on a patient’s “antigen presentation machinery,” or APM.
The APM describes how well the body flags cancer cells and presents them to the body’s immune system for destruction – a key function for checkpoint inhibitors to be effective.
Better insight into exactly who would benefit from the drugs would allow physicians to avoid their use in patients who are unlikely to benefit, sparing those patients severe and unnecessary side effects.

“This is hypothesis-generating research,” said Dr. Karin Rodland, one the corresponding authors and a cancer biologist at the Department of Energy’s Pacific Northwest National Laboratory. “It’s like the moon mission, where the crew brought back rocks for study by many other scientists. Here, we are providing the raw information for scores of scientists to pore over, to study and to generate new hypotheses. Eventually we hope this information will lead to clinical trials and perhaps new ways to treat this disease.”
The team has made all the data accessible to researchers in a web tool called LinkedOmics, which also provides computational tools for further exploration of this dataset. “This resource will enable broad usage of the data for new discoveries in endometrial cancer research,” Zhang said.
Read all the details of this study in the journal Cell.
This work was supported by grants U24CA210955, U24CA210954, U24CA210972, U24CA210979, U24CA210986 and U01CA214125 from the National Cancer Institute’s Clinical Proteomic Tumor Analysis Consortium (CPTAC), by grant RR160027 from the Cancer Prevention & Research Institutes of Texas (CPRIT), and by funding from the McNair Medical Institute at the Robert and Janice McNair Foundation. The measurements of proteins and protein activity were done at EMSL, the Environmental Molecular Sciences Laboratory, a user facility funded by the DOE’s Office of Science and located at PNNL.