Immune checkpoint therapy for ER+ breast cancers, a missed opportunity?
In the United States, apart from some forms of skin cancer, breast cancer is the most common cancer in women. It is also the most common cause of death from cancer among Hispanic women and the second most common among all other women, after lung cancer. There are different types of breast cancer, and for this reason there are multiple alternative treatments. Determining a patient’s specific cancer type helps physicians decide which of these therapies are most appropriate.
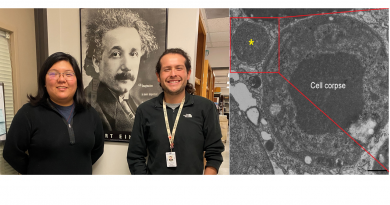
At Baylor College of Medicine, Dr. Meenakshi Anurag and her colleagues apply precision data science to improve breast cancer diagnosis, treatment and survival. In a recent study, the researchers studied estrogen receptor positive (ER+) breast cancer, a type that represents nearly 75 percent of breast cancer cases.
“Endocrine therapy has dramatically improved outcomes for ER+ breast cancer patients; however, about one-third of cases do not respond to this therapy,” said Anurag, assistant professor of medicine at Baylor and first and co-corresponding author of this work. ““Here we focus on ER+ breast cancers that are resistant to endocrine drugs such as aromatase inhibitors.”

ER+ breast cancer can be divided into two subtypes: luminal A and luminal B. The latter type is more aggressive, showing greater tumor proliferation rates and worse patient survival, when compared with luminal A type.
“In clinical trials, almost 50 percent of women with luminal B respond poorly to endocrine therapy,” Anurag said. “This result motivated us to search for tumor characteristics that could be modified in order to make the cancer more susceptible to therapy.”
Searching the genome
To search what could make these cancers more susceptible to therapy, the researchers conducted an unbiased genome-wide profiling analysis. With this type of analysis they looked to identify genes, among the 20,000 in the genome, that were more active in tumors resistant to endocrine therapy, when compared to tumors susceptible to the treatment.
“At the outset, we didn’t know what we were going to discover in this process. The transcriptome-wide profiling analysis allowed us to identify any gene that could potentially be involved in poor outcome,” Anurag said.
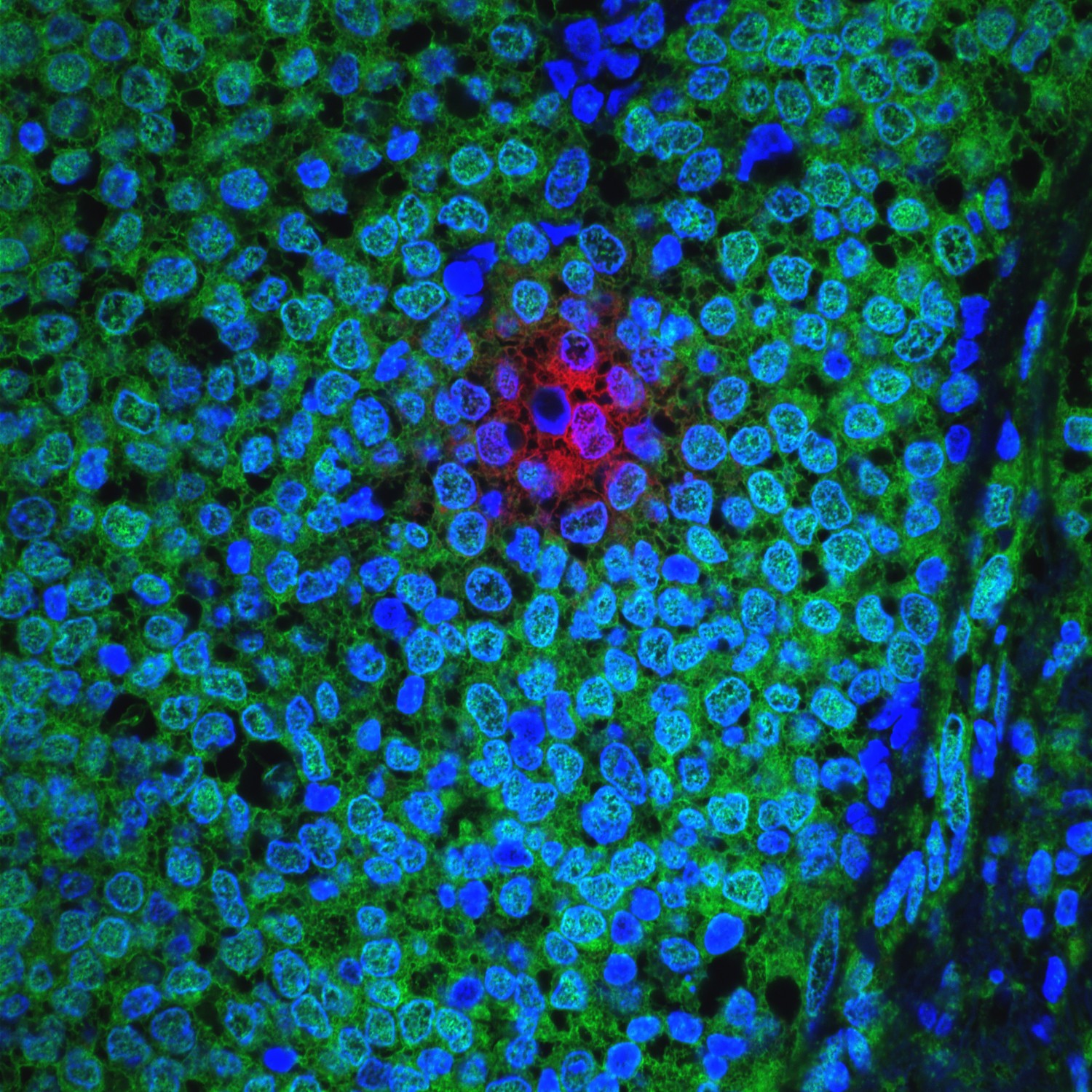
Anurag and her colleagues studied 66 luminal B cases, half of which were resistant to endocrine therapy. They found that genes that were most commonly actively expressed in resistant tumors were immune checkpoint genes, which are regulators of the immune system. These genes produce proteins that normally keep the immune system in check, preventing T-cells, a type of immune cell, from indiscriminately attacking other cells.
In some cancers, activation of immune checkpoint genes can also keep the T-cells from killing cancer cells. The gene IDO1, an immune checkpoint component, was the gene that associated the most with luminal B, endocrine therapy-resistant cancers.
“This finding is important because we know that immune checkpoint pathways can be manipulated with drugs called immune checkpoint inhibitors,” Anurag said. “Inhibiting immune checkpoints in cancer is like removing the ‘brake’ that is keeping the immune system from attacking the tumor.”
An unforeseen possibility
This study is significant because it’s been thought that ER+ breast tumors will not respond to immunotherapy, Anurag explained. “But we have shown that a subset of endocrine therapy-resistant luminal B breast cancers activate immune responses that could be amenable to manipulation with immunotherapy,” Anurag said.
“This paper identifies an important missed opportunity – the treatment of aggressive ER+ breast cancer with immune checkpoint therapy. While the current emphasis for immunotherapy is almost entirely on triple-negative breast cancer, we think that this focus excludes as many as half of the patients who could benefit, because endocrine therapy-resistant luminal B disease is as common as triple-negative breast cancer,” said co-corresponding author, Dr. Matthew Ellis, professor and director of the Lester and Sue Smith Breast Center, associate director of precision medicine at the Dan L Duncan Comprehensive Cancer Center and McNair Scholar at Baylor.
“Our findings highlight the importance of personalized medicine. Proper stratification of patients before treatment would help identify individuals who are likely to respond to treatments targeting immune checkpoints,” Anurag said.
Find all the details of this study in the Journal of the National Cancer Institute, and learn in From the Labs about previous work by Anurag and colleagues regarding DNA repair defects that may help identify an elusive form of breast cancer.
Other researchers who contributed to this work include Mayanne Zhu, Chen Huang, Suhas Vasaikar, Junkai Wang, Jeremy Hoog, Samantha Burugu, Dongxia Gao, Vera Suman, Xiang H Zhang, Bing Zhang and Torsten Nielsen. The authors are affiliated with one or more of the following institutions: Baylor College of Medicine, University of British Columbia, The University of Texas MD Anderson Cancer Center Houston, Washington University School of Medicine Saint Louis and Mayo Clinic.

Support for this project was provided by Susan G. Komen Promise grant (PG12220321), Cancer Prevention and Research Institute of Texas (CPRIT) Recruitment of Established Investigators award (RR140033) and Clinical Proteomic Tumor Analysis Consortium (CPTAC) (U01CA214125). Further support was provided by the National Cancer Institute of the National Institutes of Health (Award Numbers U10CA180821, U10CA180882 and U24CA196171, R01 CA095614, U10CA180833, and U10CA180858). The Z1031 trial also was supported, in part, by funds from AstraZeneca, Novartis Pharmaceutical Corp. and Pfizer Inc.