From chick to bedside: Removing the Wnt barrier
By Ruth SoRelle, M.P.H.
Kick starting a process that might repair the damage done in cerebral palsy and multiple sclerosis could begin with disabling a driver that helps block regeneration, said Baylor College of Medicine researchers in a report that appears in the journal Neuron.
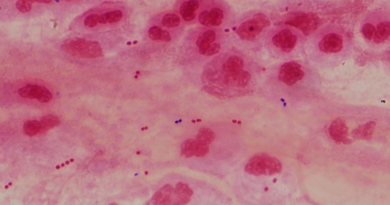
When an infant is deprived of oxygen during or shortly after birth, the brain’s white matter – home to the myelin-making oligodendrocytes – is damaged. Without myelin, the messages between nerve cells are interrupted or slowed. Similarly, the myelin sheath that covers nerves degenerates in multiple sclerosis, again interrupting the message that travels from neuron to neuron.
Increasing cerebral palsy
Cerebral palsy is increasing in recent years, with approximately 12,000 cases diagnosed annually.
As more infants’ lives are saved at earlier stages in the development, the risk of damage from lack of oxygen to the white matter of the brain increases. That kind of injury is the cause of cerebral palsy.
 “Yet, those lesions in the white matter are populated by oligodendrocyte progenitors sitting in suspended animation,” said Dr. Benjamin Deneen, associate professor in the Stem Cells and Regenerative Medicine Center at Baylor and the Center for Cell and Gene Therapy at Baylor, Texas Children’s Hospital and Houston Methodist Hospital and corresponding author of the report. “The cells that are supposed to be making myelin are not doing it. If you could coax those cells to differentiate, you might have something.” Cells that differentiate are mature and can carry out their prescribed function(s).
“Yet, those lesions in the white matter are populated by oligodendrocyte progenitors sitting in suspended animation,” said Dr. Benjamin Deneen, associate professor in the Stem Cells and Regenerative Medicine Center at Baylor and the Center for Cell and Gene Therapy at Baylor, Texas Children’s Hospital and Houston Methodist Hospital and corresponding author of the report. “The cells that are supposed to be making myelin are not doing it. If you could coax those cells to differentiate, you might have something.” Cells that differentiate are mature and can carry out their prescribed function(s).
Previously, collaborators at the University of California San Francisco had shown that Wnt signaling pathways are present at high levels in oligodendrocyte precursors, and Wnt blocks the ability of cells to differentiate.
How did the Wnt signaling pathway get involved?
Dr. Hyun Kyoung Lee, a postdoctoral fellow in Deneen’s laboratory at Baylor, began to uncover the answer, using chicks and their development as an experimental model.
“We knew a protein called Daam2 is important for Wnt signaling and receptor clustering of the Wnt complex,” said Lee. “How does it do that?”
Using a variety of techniques including a hypoxia chamber that caused damage to the white matter, she and her colleagues showed that Daam2 interacts with another protein called PIP5K(inase) to allow the clustering that promotes Wnt signaling and prevents differentiation of the oligodendrocyte precursor.
In studies in two different mouse models – one that mimicked the damage of cerebral palsy and the other, multiple sclerosis – they found that those mice that lacked Daam2 had accelerated oligodendrocyte differentiation during development. In addition, the lack or reduction in activity of PIP5K (which interacts with Daam2 at the membrane level) also reduces differentiation of the oligodendrocyte precursors.
They also found that Daam2/PIP5K are expressed in the “suspended” oligodendrocyte precursors in the human neonatal brain after hypoxic injury, directly implicating this mechanism in neonatal white matter injury.
Drug inhibitor
When they used a drug that inhibited PIP5K in a mouse brain injury model activated by a lack of oxygen, they saw differentiation of the oligodendrocyte precursors and increased myelination or formation of the nerve sheath.
While the drug could not be used in people, this finding presents a target for future drug development, said Deneen.
“There is no current treatment for cerebral palsy,” said Deneen. “We need to find a drug that interrupts the Daam2/PIP5K interaction.”
Deneen is also a member of the Jan and Dan Duncan Neurological Research Institute at Texas Children’s Hospital and Baylor.
Others who took part in the research include Lesley S. Chaboub,Wenyi Zhu, Daniel Zollinger, Matthew N. Rasband,all of Baylor, and Stephen P.J. Fancy of the department of neurology at the University of California San Francisco.
Funding for the research came from the National Multiple Sclerosis Society (Grant RG 4623A1/2 to B.D., TA 3054-A-1 to H.K.L.), the Sontag Foundation (B.D.), the National Institutes of Health (Grants R01 NS071153 to B.D. and R01 NS044916 to M.N.R.), the Baylor College of Medicine Intellectual and Developmental Disability Research Center (Grant HD024064) and by the Integrated Microscopy Core at Baylor College of Medicine, with funding from the NIH (Grants HD007495, DK56338, and CA125123), the NCI Designated Dan L. Duncan Cancer Center, and the John S. Dunn Gulf Coast Consortium for Chemical Genomics.