Mutated genes and rogue proteins can reveal new ways to treat breast cancer
Scientists are puzzled by mysteries such as, why a certain drug that induced one tumor to shrink in one patient did not affect the growth of a similar tumor in another patient? Each person’s cancer has a particular molecular signature that drives tumor growth, and identifying this signature can lead to personalized treatments that potentially neutralize these specific biological drivers, destroying the tumor or stopping it from growing and spreading to other parts of the body.

The molecular signature refers to the mutated genes and their rogue proteins whose activity changes the normal workings of the cells to a cancer-prone activity. To identify personalized cancer therapies, a team of researchers at Baylor College of Medicine, Washington University School of Medicine in St. Louis and the Broad Institute of MIT and Harvard, first search for the proteins that drive tumor growth, and then test in the lab drugs that potentially neutralize these specific biological drivers.
“Here we study the problem of how to design more effective cancer treatments with a two-pronged approach,” said co-senior author Dr. Matthew Ellis, professor and director of the Lester and Sue Smith Breast Center and McNair Scholar at Baylor. “We combine patient-derived xenografts and proteogenomic integration.”
Patient-derived xenografts: a human tumor model in a ‘living container’
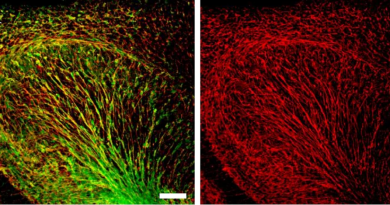
A patient-derived xenograft consists of a sample of a human tumor transplanted into a particular laboratory mouse.
“We grow human tumors direct from patients in laboratory mice because we want to mimic the living natural environment tumor cells grow in – a beating heart, blood vessels and other biological structures – that is as natural as we can possibly make it. We think this approach offers a closer representation of the tumor’s growth environment to study cancer drugs than cells growing on a laboratory plastic dish,” Ellis said.
In previous studies, the researchers showed this approach can be successful as patient-derived xenografts of breast tumors recapitulate most of the genes expressed and the proteins present in the original breast tumors. In addition, responses of breast cancer patient-derived xenografts to drug treatments resemble that observed in the corresponding patient. These results suggest that patient-derived xenografts of breast tumors are potential useful models in which to identify and test targets for breast cancer therapy.
Proteogenomic integration: looking at proteins and genes together
Cancer cells may not only be different from normal cells in the types of genes they express but also in some of the proteins they use to carry out their functions. Some cancer proteins can drive normal cells into a path that leads to cancer and identifying and neutralizing these biological drivers may result in better treatments. Proteogenomic integration allows researchers to look at the proteins present and the genes expressed in the tumor, side by side.

“Proteins carry out most of the biological functions in the cell,” said co-senior author Dr. Li Ding, an associate professor of medicine at Washington University School of Medicine in St. Louis. “Knowing the DNA sequence of genes does not automatically tell us everything about the proteins doing work in the cells.”
“Identifying the rogue proteins of cancer is an important pathway toward developing new drugs,” said co-author Dr. R. Reid Townsend, professor of medicine and director of the National Institutes of Health / National Institute of General Medical Sciences Biomedical Mass Spectrometry Resource at Washington University.
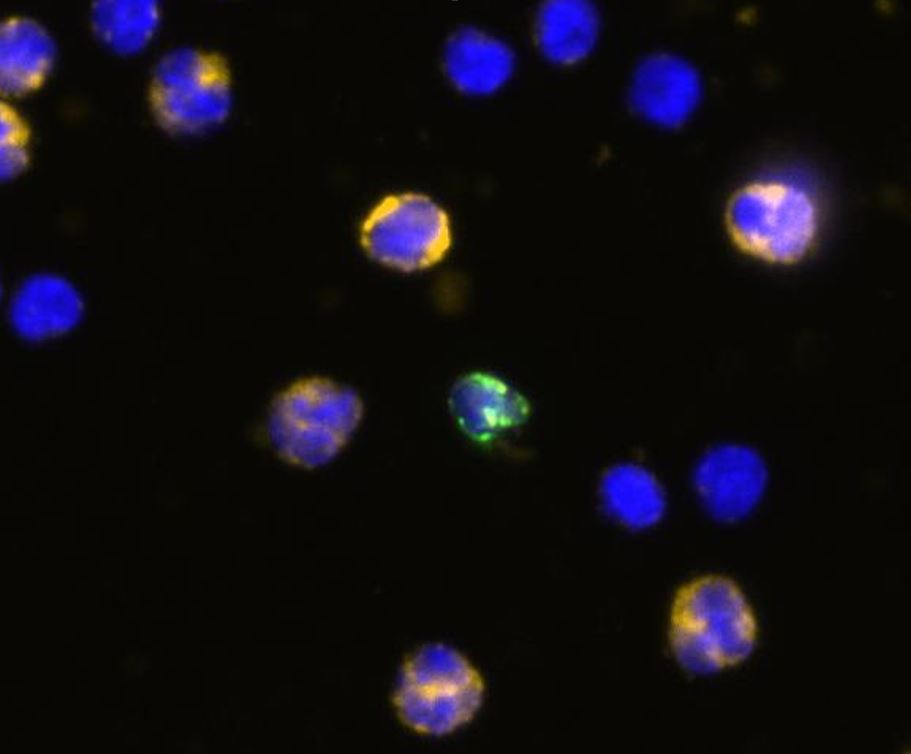
In this study, the researchers used mass spectrometry, a leading method for detecting, quantifying and characterizing proteins, to determine the proteins present in each of 24 patient-derived xenografts of breast tumors representing different breast cancer subtypes. In total, they identified nearly 10,000 proteins and their relative abundances across tumors.
“A substantial number of these proteins identified in the xenograft model are potential targets for drugs,” said Ellis. “In addition, similar protein signatures were observed in breast cancer samples from patients, which suggests our approach has potential clinical relevance.”
In selected patient-derived xenografts of breast tumors in which the researchers observed certain ‘rogue proteins’, targeting those proteins with specific inhibitors resulted in suppression of tumor growth in the xenograft model, thus validating their two-pronged approach to cancer treatment.
“The idea behind this approach is to find out what are the driving pathways of each person’s cancer,” Ellis said. Once we know these pathways, the next step is to use drugs to interrupt these pathways and lead to outcomes that are better than giving patients non-specific therapy. The mouse work is promising enough to adapt these technologies for real time analysis of patient samples so that clinical trials can be designed to test this new diagnostic and drug selection approach. The National Cancer Institute has agreed to invest in this next phase of the project.”
Read all the details of this study in Nature Communications.